This post is "live" and ongoing. It will be continually updated.
To follow this post, bookmark it in your browser, return to this page at a later date using the bookmark, then refresh the page in your browser and scroll to the bottom to see the updates.
To see an ongoing list of out-of-pocket expenses I've paid, scroll to the bottom of this post to see the section entitled "Out-of-pocket Medical Expenses."
Overview
According to the Mayo Clinic website:
Dysphagia is a medical term for difficulty swallowing.
Symptoms include:
- Pain while swallowing.
- Not being able to swallow.
- Feeling as if food is stuck in the throat or chest or behind the breastbone.
- Drooling.
- Hoarseness.
- Food coming back up, called regurgitation.
- Frequent heartburn.
- Food or stomach acid backing up into the throat.
- Weight loss.
- Coughing or gagging when swallowing.
Source:
"Dysphagia". Mayo Clinic. Retrieved 2023-11-05
Swallowing is an essential bodily function providing our bodies with a way to ingest all of the nutrients we need to survive. Like breathing, we take the ability to swallow for granted. Until the summer of 2022 I had never heard of the word "dysphagia" but as time progressed I would become intimately familiar with it.
As my dysphagia slowly progressed, I did a ton of online research. I came to understand that there are a lot of things that can cause it, and that diagnosis isn't simple or easy.
Initially, because I had ongoing, supposed allergies for a number of years (which I was addressing with a daily allergy pill and saline sinus flushes), which manifested as a slow, steady flow of thick mucous down the back of my throat, I thought that maybe the constant flow of mucous was irritating my throat, causing inflammation and swelling. This "working theory" was never confirmed by what doctors were telling me, but doctors weren't giving me any definitive answers.
The next "working theory" was that I had something called LPRD (Laryngopharyngeal Reflux Disorder), a type of acid reflux where stomach acid somehow manages to work its way up into your throat. Symptoms of LPRD include continual throat clearing, dysphagia, chronic throat irritation, excessive phlegm in your throat, and post-nasal drainage.
In December of 2022 I started having pain in the back of my head (occiput, left side). At first it was barely noticeable, but as time progressed it became slowly more pronounced, especially when swallowing.
Up to this point, everything I had read, combined with what I was (and was not) being told by doctors, led me to believe that most likely I had some kind of nerve problem. In particular, I suspected the vagus nerve.
According to the Cleveland Clinic website, signs of vagus nerve problems are "acid reflux" and "difficulty swallowing" (among others). I suspected that something was pressing against my vagus nerve somewhere in my cervical spine.
Another "working theory" was that I had some other type of neuralgia, of which there are several, possibly Occipital Neuralgia.
Before I launch into a chronological account of my journey with this debilitating condition, I need to say something about how long it took for me to get any definitive answers from the medical community.
Until just recently (mid-October, 2023), the word "cancer" wasn't mentioned in conversations I had with doctor, after doctor, after doctor. As you'll see, what started as several mentions of swallowing difficulty to my Primary Care Physician (PCP) over the course of more than one year, followed by appointments with a gastroenterolgist, then with an ENT (Ear, Nose, and Throat doctor), then a neurologist, then with a chiropractor, then with a spine surgery and orthopedic clinic, then with two other ENT's finally ended up with a cancer diagnosis. Add to that five separate visits to my PCP in 2023 (February, March, May, June, and July).
According to the Mayo Clinic website "difficulty swallowing" and "a sore throat" are two symptoms of throat cancer.
I expressed these two symptoms multiple times to my PCP, to the gastroenterolgist, to the ENT, to the neurologist, to the chiropractor, to the orthopedic clinic, and to the second ENT. It wasn't until my visit at the orthopedic clinic that I began to understand what was really going on with me.
In addition to swallowing difficulty, the head pain I was experiencing, especially when swallowing, continued to slowly get worse. Of course, I expressed this symptom as well to all of the aforementioned doctors, who led me to believe that my condition was due to allergies, the disc degeneration in my neck, a neuromuscular problem, or possibly related to acid-reflux.
How much more information does a doctor need before a "red flag" appears?
A simple CT Scan and/or an MRI of my throat (cervical spine) back in March or April of this year, in all likelihood, would have shown there was something of concern going on. As everyone knows, early cancer detection is often the key to successful treatment and survival.
You might wonder why I myself didn't consider the possibility of cancer. It's a good question, and looking back it's clear that I should have. Hindsight is always 20/20, right? But I'm not a doctor, and as I've said, I was being led in other directions by all of the doctors, and none of those directions included cancer. Add to that the fact that I've never smoked, never chewed tobacco, and have never done any kind of recreational drugs (not even Marijuana). Cancer just wasn't on my "radar."
Yes, I'm disappointed, frustrated, and angry with how long it took to finally get some answers. It's inexcusable, and in my opinion a complete failure of our health care system.
If you have any dysphagia symptoms, I urge you to request imaging (CT Scan and/or MRI) of the cervical spine (neck) at the outset. Don't count on your doctor to bring this up, request it yourself, and if your doctor refuses, see another doctor who will.
If you choose to read my chronological account below, you might ask yourself how I was able to remember all of these details. I've been keeping a medical journal of all my doctor visits and procedures for a long time, and that, along with my memory (which is quite sharp) is the source of the information.
You might also wonder why I've gone to such great lengths to document this. It's quite simple. Reviewing what's transpired and documenting it is a way for me to process what's happening now and all that's happened that got me to this point. It's a way of examining, clarifying, and yes, venting so I can move forward with what's ahead.
Early 2021
In February of 2021 I first mentioned I was having some difficulty swallowing to my PCP. At that time the difficulty was very infrequent. My PCP told me to let him know if it continues or gets worse.
For the next year or so my mild swallowing difficulty continued, but still not frequently or severe enough to be a concern.
Summer, 2022
In late July I saw my PCP again complaining of a sore throat and continued difficulty in swallowing. He checked my throat and sinuses, then told me it was just allergies.
Fall, 2022
By late September of 2022 my swallowing difficulty had become more frequent and worse. This time my PCP sent me to see a gastoenterologist.
In mid-October I saw a gastroenterologist at Scottsdale Gastroenterology Specialists for a consultation. He said he wanted to do an esophagogastroduodenoscopy (EGD, also know as an Upper GI). Basically, an EGD is where they maneuver a long cord with a camera attached to the end down your esophagus, into your stomach, and into the upper part of your small intestine looking for any abnormalities.
In mid-November I had the EGD completed. It didn't show any major problems or anything that might be related to swallowing difficulty. Despite that result, my gastroenterologist had me take a stomach-acid blocker called Pantropazole (generic for Protonix) for 7-8 weeks to see if it had any effect on my dysphagia. I took the Pantoprazole for 52 days. It seemed to decrease my symptoms a bit, but because my swallowing difficulty varied from day to day within a range, I couldn't say that it had a significant overall effect. It seemed that if it was really helping the effect would have been more dramatic and noticeable. The other reason I stopped taking it is because I wanted to see if it was causing my head pain (one of its side effects).
My gastroenterologist also recommended I make an appointment with an ENT.
Early 2023
In mid-January I saw an ENT at Valley ENT. He used an endoscope to look at my sinuses and throat. He didn't see any "smoking gun" and he wasn't able to tell me where the thick, constant, slow flow of mucous down the back of my throat was coming from.
The ENT ordered a CT Scan of my sinuses. He also ordered a Modified Barium Swallow Test.
Other than a deviated septum (very common), the CT Scan showed nothing else of concern.
The Swallow Test showed that my hyoid bone was not elevating properly and that the muscles in my throat, including my UES (Upper Esophageal Sphincter) might be weak . The conclusion was "mild pharyngeal dysphagia."
I was also given a handout going into great detail about LPRD and how to treat it.
I read the handout and implemented many of the suggested "lifestyle" changes, elevating the head of my bed three inches, reducing my intake of certain foods, and being very careful to not lie down after meals for at least two hours after eating.
I distinctly remember having a conversation with the ENT about all the possible causes of my dysphagia. I asked him if maybe I had a low-grade bacterial infection, or possibly a virus. He added that it could also be something called oral thrush. He concluded our conversation by saying that he was "not ruling anything out."
When I mentioned my head pain, he seemed genuinely perplexed, and gave me a referral to a neurologist.
It wasn't until some time had passed that I thought back on this conversation and asked myself the following questions:
- Why didn't this doctor put me on an antibiotic to see if that had any impact?
- Why didn't this doctor treat me for oral thrush?
- Why was this doctor so perplexed by my head pain? Surely I couldn't be the first patient who had reported this symptom, right?
And most importantly, why didn't this doctor order some kind of imaging of my neck (CT Scan or MRI), especially after I told him about my head pain? If you're not ruling anything out, then why on God's green Earth wouldn't you screen, right away, for the most serious, and possibly deadly condition, cancer?
I saw this ENT three times within the course of about six weeks. On my third visit (February 27), where we discussed the results of the Swallow Test and he ordered swallowing therapy for me. I had eight sessions of therapy at HonorHealth over the course of the next 2-3 months. It helped me manage my swallowing difficulty, but it did not improve it.
The ENT also said he wanted me to have a Esophageal Manometry test performed.
Before calling to schedule the test, I did some research on Esophageal Manometry. I had a hard time understanding why I needed this test because my swallowing difficulty was only in my throat, not in my esophagus. Once food got past my throat I had no problems with it getting "stuck" further down. I also found it hard to believe that my head pain had anything to do with my esophagus. I understood that the test would give us a glimpse into the PH value in my esophagus (which would help to determine if I had LPRD), but honestly, I felt the ENT was going on a "fishing expedition" because he hadn't been able to give me any concrete answers after three visits. I opted to not have the test done at this time and to see the neurologist first.
It's accurate to say that I did not have a very good rapport with this ENT. We didn't connect very well. If he had explained to me his overall strategy and plan, and addressed the concerns I just mentioned above right away, maybe my experience with him would have been different.
On February 2 I saw my PCP for ongoing head pain. He ordered a CT Scan of my brain. The CT Scan showed nothing of concern.
March, 2023
On March 3 I saw my PCP again. I complained of a very sore, inflamed throat and ongoing head pain.
I asked about having my throat cultured but my PCP said that cultures aren't very accurate because there are so many kinds of bacteria in our mouths, even among completely healthy people.
Instead, he prescribed an antibiotic, Ciprofloxin, which I took for 7 days. It didn't help with my sore throat or head pain.
At that same appointment I asked my PCP if it's possible I have meningitis. He said if I did I would already be dead.
I expressed my concern that what I have is not a typical headache, but an ache in a specific area. He seemed somewhat defensive, saying he has already ordered (and I’ve completed) the CT brain scan. Basically, he said there was nothing else he could do for me regarding my head pain. It's interesting that rather than asking more questions about my head pain he became defensive. Honestly, I was wondering whether he thought I was just "imagining" the pain in my head, or whether he just, for whatever reason, was fed up with my same old "story."
May, 2023
On May 4 I had my first appointment with a neurologist at HonorHealth Neurology. Yes, that's about two months after getting a neurologist referral from the ENT, but that was the soonest available of all the neurologists who practice there.
Because I was still thinking my dysphagia and head pain were most likely a nerve issue, I had hope that seeing a neurologist would help me get to the bottom of it.
He said that my dysphagia was not a nerve issue because if it was, then swallowing liquids would be a major problem (my swallowing problem was only with solid food).
The neurologist ordered an MRI of my brain, with contrast.
On May 9 I saw my PCP again. I asked him to prescribe something for oral thrush. I didn't have any of the oral thrush symptoms, but this was a way of "ticking off another box" of possible conditions. My PCP prescribed Nystatin - a liquid you gargle with, then swallow. I tried it for one day and decided it was just too unpleasant to swallow.
During that same visit I expressed my concern to my PCP about my recent weight loss. He said it's normal to lose weight as we age, but normally not until approaching age 80 (I'm 69). He suggested I drink two bottles of Ensure each day to address it. I wasn't aware of it at the time, but acccording to the Mayo Clinic website "weight loss" is a symptom of throat cancer.
June, 2023
On June 7 i saw the neurologist again to discuss the results of the MRI. It showed nothing of concern.
He ruled out Glossopharyngeal Neuralgia and Trigeminal Neuralgia.
The neurologist said my head pain was most likely caused by the disc degeneration in my neck/cervical spine. He said that there was nothing else he could do for me.
When I asked him for an ENT referral he gave me the name of a doctor at Scottsdale Ear, Nose & Throat. When I called and tried to book an appointment, I was told that I could not see that doctor because I had already seen a doctor at Valley ENT (Valley ENT and Scottsdale Ear, Nose & Throat are under the same "umbrella").
The neurologist did not order any imaging (CT Scan or MRI) of my neck.
On June 11 I saw my PCP again. We talked about the results of my recent brain MRI and my ongoing head pain. My PCP suggested I try some physical therapy.
I'm a big fan of PT. After three sessions it was clear that PT was not doing anything to address my head pain.
I also asked my PCP to put me on a different stomach acid medication, Famotidine (generic Pepcid), to see if that might help my dysphagia (still thinking that just maybe I have the aforementioned LPRD). He said that if the medication is working I should see results within 30 days. After 43 day with no improvement I stopped taking the drug.
July, 2023
On July 10 I saw my PCP again to discuss recent weight loss and ongoing swallowing difficulty and head pain.
I suggested the possibility of seeing a chiropractor, and my PCP agreed. I suggested getting a neck X-ray and my PCP agreed.
The neck x-ray showed nothing that pointed to head pain.
August, 2023
By this time the ache/pain in my head was worse. Eating and swallowing had become a not-so-fun experience. It's bad enough when food doesn't want to pass down your throat when you swallow and you have to exert effort (small bites, wash each bite down with water), with added head pain it was very uncomfortable.
On August 11 I saw a chiropractor who was highly recommended to me by both a friend and a neighbor. My insurance didn't cover chiropractic, but at this point I was willing to see just about anyone, hoping to get even a clue as to where to go next. I stopped in and talked to the chiropractor before agreeing to the evaluation and treatment, explaining to him everything I had already tried and who I had already seen.
Unfortunately, I felt no relief whatsoever after the treatment which included an adjustment, deep-tissue massage, and a lot of other manipulations. The doctor's intuition was that my problem was possibly acid-reflux (30% chance), musculoskeletal tension (70% chance), or something to do with the vagus nerve (which I brought up during the evaluation).
I noted in my journal that I was feeling that my tongue was laboring sometimes, especially if I had a longer conversation with someone. I also noted that some words were hard to pronounce properly (as if I had some kind of speech impediment).
I was still thinking that the most likely cause was nerve-related, in particular the vagus nerve. And, by this time I had completely given up on my PCP.
Taking the matter into my own hands (and not needing a referral from my PCP to see a specialist any more because I had just changed insurance plans), I decided to make an appointment at Sonoran Spine. I had been to Sonoran Spine a few years prior for a non-related issue and I thought highly of the nurse practitioner I had seen there.
On August 29, I saw Kelli Patterson, FNP-C (certified family nurse practitioner) at Sonoran Spine and explained in great detail what I was experiencing and what I had already been through. She didn't have any answers for me on this visit, but she suggested we get a current MRI of my cervical spine. She also said she would have a conversation with the doctor who she works for, Spine Surgeon Dr. Michael Chang, to see if he had any ideas.
About a week prior I logged the following in my medical journal:
Over the past few weeks my head ache/throb has gotten progressively worse. It’s very painful to eat meals and the pain seems to be there almost all of the time at some level of discomfort. The pain is still in the same spot, left occiput area, which radiates to my left temple and behind my left eye. The pain is always the worst when I eat and swallow.
Also, I'm noticing that it hurts when I brush my teeth (same head pain) and sometimes when I push my tongue to the left side of my mouth. And, it feels like talking/speaking is just a little difficult and occasionally words don't come out perfectly.
September, 2023
While waiting for my scheduled MRI, I decided to see a different ENT in order to get another opinion.
On September 15 I saw a Physician's Assistant (PA) who works for ENT Dr. Brian Lee at the Scottsdale Sinus and Allergy Center. I explained my symptoms to her and gave her a brief history of everything and everyone I had already tried and seen.
An endoscope of my sinuses showed enlarged "nasal turbinates" and a lot of mucous (in my upper sinuses as well). The PA wanted Dr. Lee to do procedures to address these two issues, but she agreed that those issues were not contributing to my throat, swallowing, and head pain issues. I opted to not have those procedures done.
The PA also ordered blood work done to check for both food and airborne allergies. The result of that blood work showed no food allergies, but moderate allergies to several different grasses and a certain type of thistle.
The PA did not order any imaging (CT Scan or MRI) of my neck.
I asked to book an appointment with Dr. Brian Lee. The soonest available appointment was November 21, which I booked.
October, 2023
On October 3 I had a follow-up visit at Sonoran Spine with Kelli Patterson to discuss the results of the Cervical Spine MRI. My spine itself showed nothing of concern, but the following was noted:
The partially imaged oral cavity demonstrates heterogeneity and masslike enlargement localizing to the right lingual tonsils/root of the tongue worrisome for neoplasm.
A neoplasm is an "abnormal and excessive growth of tissue."
Thinking it would show more detail, Kelli ordered a Cervical Spine CT Scan, which I had completed on October 13.
Early the next week, I received a voice message from Kelli saying the results of the CT Scan showed reasons for concern. Essentially, the scan showed I had a growth at the left base of my tongue (suspected extension to the right side as well), and two other growths near lymph nodes on my neck (one on the right and one on the left).
Sonoran Spine gave me a referral to a different ENT to discuss these new findings.
On October 19 I saw an ENT at Enticare. After reading the results of the CT Scan and hearing my long-winded story of all the doctors I had been to previously, she endoscoped my sinuses, then gave me a list of referrals to head and neck oncology doctors. She also said she was surprised that someone had not discovered this much earlier.
I reviewed the list and immediately called the Banner MD Anderson Cancer Center in Gilbert. I was booked with an appointment at Banner's Rapid Access Clinic to see a nurse practitioner the following week.
On October 24 I saw the nurse practitioner. I provided her with a two-page document describing my ongoing symptoms and every doctor I had previously seen. She said she would have the schedulers get me in to see an oncology head and neck surgeon ASAP.
Two days later on October 26 I saw Dr. Pardis Javadi, one of four head and neck oncology surgeons at Banner MD Anderson.
She endoscoped my sinuses and throat. We were able to see that the mass growing at the base of my tongue was pushing upwards in the back of my mouth. I asked her if it was possible that the growths were not cancer. She said that if I were much younger the chances were good, but at my age it's most likely cancer. She ordered a biopsy.
November, 2023
On November 2 a biopsy was performed on the growth on the left side of my neck near a lymph node.
On the evening of November 7 I was able to view the biopsy report on my Banner patient portal. The results read:
Positive for malignant cells.
The cytologic findings favor metastatic squamous cell carcinoma.
Not the result I was hoping for, but what I was expecting based on what Dr. Javadi had said.
Two days later on November 9 I had a follow up phone conversation with Dr. Javadi. She confirmed the biopsy report. When I asked about the possibility of surgery she said that was not an option because it would severely degrade my quality of life (possible damage to my vocal cords, the use of my tongue, and my ability to swallow).
She said the path forward would be a combination of radiation and chemotherapy.
She submitted an order for a Pet Scan (positron emission tomography) in order to determine where else in my body there might be cancer cells growing.
In addition, I was scheduled for a meeting with my oncology team on November 16 (the day after the PET Scan).
Not knowing if I had cancer cells in other parts of my body was stressful and unnerving, to say the least. I sensed an urgency to have the PET Scan completed within days, not weeks (which is sometimes the case with scheduling) for my own peace of mind, but even more importantly so the oncology team had that information so they could complete my treatment plan. Without it, because of the way Banner schedules oncology teams meetings (only on Thursdays), and because of the upcoming Thanksgiving holiday the following Thursday, not having the Pet Scan report might have delayed my treatment an additional two weeks - not something I wanted to happen.
Luckily, or more precisely because I intervened and spent many hours on the phone on two different days pleading my case, on November 15 I had the PET Scan.
The following morning on November 16 I downloaded the report. To my relief the report showed that the cancer was confined to my neck and throat and was no where else in my body.
Later that day I met with my oncology team at Banner.
I was told I have Stage 3 cancer (T4, N2, M0). If the Pet Scan had showed cancer in other parts of my body, I would have been at Stage 4.
I was told that my cancer most likely started in my throat/tonsil area and was most likely caused by the human papillomavirus (HPV). Read more about HPV and cancer on the World Health Organization website here.
Because my P16 marker is positive my prognosis is better, and overall my prognosis for survival is good.
Treatment will consist of concurrent radiation and chemotherapy. Radiation treatments will be over a seven week period (5 days a week, 35 total). Chemotherapy will be once a week for seven weeks.
At the 5-6 week point of treatment, my throat will be very sore from the radiation and it's possible I won't be able to swallow, requiring a temporary feeding tube inserted into my stomach.
The radiologist said the treatments might result in tongue weakness and they might have some impact on my ability to swallow. I already have some tongue weakness and I've been having trouble pronouncing some words (that's been going on for the past couple of months). Hopefully, the final outcome will be no worse than where I'm at now, but I don't think they know for sure.
Other possible side effects are tightness in my neck muscles, loss of taste (2-6 months), dry mouth (salivary glands will shut down) for at least 4 months, possible partial closure of my carotid arteries over time (I will need to have them scanned every 3 years), and a chance I might need to increase my thyroid medication.
Today, I decided to start taking a pain medication called traMADol for my head pain. I had requested something for pain a couple weeks ago but was resistant to taking it because I hate taking prescription drugs unless they are absolutely necessary. The head pain I've been experiencing sometimes reaches a level 7 (where level 10 is max) - that usually happens when I eat and swallow. When it's at that level it makes my head throb.
On November 17 I had another Modified Barium Swallow Test performed. The results of that test showed that a) I was sometimes aspirating a small amount of food and liquid down my trachea (windpipe) when I swallow, and b) that the saliva, mucous, and food mixture that was pooling in my throat after swallowing was most likely because certain muscles in my tongue were not able to help force the food down my throat.
The technician who performed the test said that aspiration could be a serious problem for me in my upcoming cancer treatment. She said it could result in pneumonia, which, obviously, in the middle of a weeks-long treatment program would be a major problem.
She also said that as the weeks of my treatment progressed, my swallowing difficulty might get worse due to swelling. If that happened, it would be even more difficult for me to ingest a reasonable amount of food and maintain proper nutrition (at this point I had lost 5-7 pounds over the course of a year or so).
And, because I had stopped taking large pills (like multi-vitamins) a couple months prior (because they would sometimes get stuck in my throat, causing me to choke), she said I might have a problem swallowing critical medications I would need in my treatment.
For that reason she recommended I have a feeding tube inserted into my stomach in a procedure called a Percutaneous Endoscopic Gastrostomy (PEG).
Having to use a feeding tube was something I was hoping to avoid, but the wise and reasonable thing for me to do at this point was just surrender to the fact that this was something I needed to do.
Today, November 19, I'm happy to report that the traMADol has significantly reduced my head pain. I'm taking two 50mg tablets daily (max is four/day). The only side effect so far is constipation, which, as of yesterday, I'm addressing by eating prunes.
Today, November 20, I completed my last workout at L.A. Fitness before surgery tomorrow. Those of you who know me well know that not being able to workout the way I'm used to (or maybe not at all, depending on how I feel) is going to be a HUGE blow to my mental, emotional, and yes spiritual health. I have depended on physical fitness for health and vitality since my mid-twenties (that's almost 45 years!). Working out energizes and calms me (all at the same time), in addition to all of the positive physical effects.
On November 21 I had the feeding tube and the port for chemo surgically implanted. I will need the feeding tube only if I am unable to eat and swallow. Right now I'm still eating some of my usual diet (but lesser portions and mostly softer foods), but as treatments start, I may need to use the feeding tube for a period of time in order to maintain weight and adequate nutrition.
Being in the the hospital for most of the day (my procedure was delayed by 2.5 hours because the surgeon ran late on a patient), the magnitude of what's happening is really starting to sink in. Beyond the physical, it's going to be a huge mental and emotional challenge for me.
Today, an appointment was booked for me to see a Dietician at Banner on Monday (November 27).
On November 22 I had an appointment to see my dentist for a checkup, cleaning, and to get impressions for fluoride trays, which I will have to use daily to help counteract the effects of radiation on my teeth. I've taken really good care of my teeth over the years, so that should help in minimizing the damage done by radiation.
The other big concern with radiation is that it can do real damage to your salivary glands, which has an impact on your teeth (saliva helps protect your teeth from acids in your mouth). The radiologist has already informed me that as radiation progresses, less and less saliva will be produced (can't say for sure how much), and I will experience dry mouth.
Also, I was told that radiation can do damage to your jawbone.
I now have an appointment scheduled for next Thursday (November 30) to do the radiation simulation. That's the last step before treatments can begin.
I received a call from someone who handles finances and billing at Banner. I was told that my portion (co-pay) for the simulation and the 35 radiation treatments will be $2,362. Because my UHC annual out-of-pocket caps at $2,500, this amount will include the 7 chemo treatments. But, taking into account that my treatments will not be completed this year, I'm wondering if this amount might not end up being more. I will need to contact UHC to find out.
Also, someone from Aveanna Healthcare delivered an initial batch of food to me today which I will use with the feeding tube (when I need it). She showed me how to use it and how to flush the tube (must do twice a day, even if I'm not using it).
After more insurance referral B.S. and several long phone calls, I decided to do all my upcoming treatments at Banner MD Anderson/Gilbert. I had informed the team about a week ago that I wanted to do all the treatments at the Banner University Medical Center/Phoenix because it was a little closer (shorter drive). But, I received conflicting information from Banner and United Health Care (UHC) about whether I needed a referral from my PCP to do that (doing my treatments at the Phoenix location would mean working with a different oncology hematologist, which Banner said would require a PCP referral). UHC said I didn't need a referral, but Banner was "adamant" that I did. And, because I had a similar situation recently, which resulted in my PCP hand-writing back to me that I do not need a referral to see a specialist (which, according to my UHC plan I do not), trying to get this waived through my PCP (to pacify Banner) would just result in the same thing and probably piss him off.
This is beyond frustrating. I shouldn't have to get involved in this. But, as has happened to me so many times over the past year or so, you just have to "take the bull by the horns" yourself and make the necessary phone calls so you can move forward.
Today, November 23, I'm having quite a bit of pain where the feeding tube was implanted. The pain started yesterday. I'm taking pain medication (traMADol 50 mg and Acetaminophen 500 mg) but I still get these short "pulses" of fairly severe pain (level 7-8) which last just a couple of seconds then go completely away. I expected some pain when moving in a way which uses my abdominal muscles (like getting in and out of bed, bending over to tie my shoes, etc.), but this seems excessive.
For whatever reason, today, November 24, I woke up with major congestion in my throat (saliva and mucous) and a very deep, hoarse voice. Because of the feeding tube surgery earlier this week, trying to clear the phlegm by coughing was very painful (you use your abdominal muscles to cough).
My biggest concern was that maybe the congestion was also in (or might move into) my lungs. Because I aspirate more than normal, lung-borne illness is a major concern for me, especially as I begin treatments. I went to my local Urgent Care. Temperature normal (I didn't feel sick). Lungs sounded OK (stethoscope). The attending PA ordered a chest x-ray, just to be sure, which I had done later in the day (PA called later, lungs OK, no fluids). They also tested for strep (negative) and COVID (negative).
Today, November 25, I still have a cough (deep in my throat), but not quite as bad as yesterday. It still hurts to cough up phlegm, a lot (and continued pain over time wears you out).
Later in the day (evening, around 8 pm) I felt my forehead -it felt very warm. I took my temperature - 102.1. Not good. And, I had really bad chills, to the point where my whole body was trembling.
I went to the HonorHealth ER. Temperature there was a little less (101.4). The attending physician tested for COVID, Influenza, and RSV (Respiratory Syncytial Virus). All test results were negative. My official diagnosis was "Fever of unknown origin."
The nurse peeled back the dressing on my feeding tube to see if anything looked abnormal. As far as she could tell, no signs of infection. The physician did a little poking around in my belly to see if I had any pain (no pain).
I was discharged from ER. On the way out I had those same trembling chills I had earlier in the evening. I was still coughing, occasionally.
Today, November 26, I'm still coughing from time to time (yes, it still hurts), temperature this morning was 98.6.
To say I'm confused and concerned doesn't even come close to what I'm feeling. I potentially have some type of "bug" or virus, I don't know what it is, and if things go as planned I will begin cancer treatments late this week or early next week. What happens if this doesn't go away as the week progresses? How might that affect my treatments? And even if it goes away, how do I know it won't come back later?
I've already discussed the dangers of acquiring a lung infection with my cousin (and retired RN) Linda. I also discussed it with the attending nurse at HonorHealth last night. Both agreed that if I were to get pneumonia during treatment, it could be life-threatening.
Today, November 27, I met with a Dietician at Banner to discuss how to use the feeding tube, ask questions about the chemotherapy, nausea, etc. All the food I will be receiving through the tube will be liquid (6 cartons per day). The plan is to keep eating by mouth for as long as possible.
I coughed up more phlegm this morning (this time it had a very pale green or brown color, temperature a little below normal). I explained to the Dietician what I was experiencing since last Tuesday with the coughing, chills, and high fever. She suggested I call the Banner nurse phone number tomorrow if I still have symptoms.
This evening I have a temperature of 101.7 at 5:30 pm, and 100.1 at 7:45 pm. Still coughing up small amounts of phlegm from time to time (seems to come and go).
Today, November 28, not long after I got out of bed I coughed up some very pale brown/yellow phlegm. Temperature was slightly below normal.
I called my assigned nurse navigator, explained what has been going on over the past 4-5 days, she said she would get in touch with my oncologist, Dr. Radhi, then call me back. I received a call back, was scheduled for blood work and a chest x-ray followed by an appointment with Dr. Radhi today.
In my appointment with Dr. Radhi (temp 97.2, weight 124.8 lbs.) I explained in great detail what I have been experiencing recently. My blood work was all OK (no elevated white blood cell count, which might indicate an infection), but they also drew blood directly from my port to make sure there is no infection in and around that area (will take few days to see if cultures show anything). My chest x-ray was clear (no fluids, no signs of pneumonia). Dr. Radhi wasn't able to give me a reason for my recent symptoms. She told me to keep monitoring them, and if they continue or get worse, to call.
I'm convinced that the phlegm is coming from my sinuses or my mouth (it's extremely salty) and then finding its way down my throat. When I cough, it doesn't feel like it's coming from my lungs (and two recent chest x-rays show no fluid or other problems).
Both the nurse navigator and Dr. Radhi were concerned that I was still aspirating. Dr. Radhi went back to look at my recent MBS Test which indicated I am aspirating a fair amount (I was under the impression that I've been aspirating less than a fair amount, based on the video images I reviewed with the technician immediately after my Test).
Dr. Radhi indicated that she wanted me to start using the feeding tube immediately and stop eating solid food and drinking water by mouth all together. I "pleaded" my case that so far I haven't had any problems from any aspiration, and that my preference was to continue eating solid food until my treatments start. She empathized with me. Honestly, I think she was right "on the fence" on this one. She reviewed the results of my MBS Test, and I think that is what convinced her to stay her course. Why this subject didn't come up with her before now is still a mystery to me (the MBS Test was completed on November 17).
I reluctantly agreed, and felt like I'd just taken another "shot to the chest." I came to this appointment to hopefully get an answer to my recent symptoms. I left with no answer, and the hard truth that I won't be eating or drinking by mouth for at least the duration of my treatments.
I asked about medications and water. I was told I can continue taking those by mouth for the moment, but I will get an update on that later in the week when Dr. Radhi's office has passed this by the team who performed my MBS Test.
Dr Radhi said that treatments usually start 5-10 days after the simulation (which is scheduled for November 30).
At 5:00 pm temperature was 97.9.
Note that after my early morning cough, I've only coughed two more times all day, both times coughing up a small amount of phlegm.
At 7:30 pm temperature was 99.9.
Lying down about an hour ago, I had to get up 3 times to cough (over 10 minutes) - coughed up that same very pale yellow (nearly clear) phlegm. After getting up, coughing and urge to cough immediately stopped. All I had before lying down was a few sips of water (no food since noon).
At 11:50 pm temperature was 96.4.
This morning, November 29, I coughed up (twice) that same slightly-colored phlegm (feels like it's deep in my throat).
I woke up last night with my skin moist from sweating. This is the fourth night in a row this has happened. It happened a couple of times before over the past couple of weeks.
Temperature at 10:30 am was 97.2.
Temperature at 11:30 pm was 98.8.
Virtually no coughing throughout the rest of the day (after this morning), but I did have to blow my nose once or twice.
No sooner do I say that, but when brushing my teeth tonight, it was like a switch had been turned on (my sinuses where clear and I felt virtually no phlegm all day, until I started to brush). As soon as I started brushing, my mouth began producing large amounts of saliva, some of which I could feel deeper in my throat (that same thick mucous I've been complaining about for over a year). And, my nose became filled with mucous (I had to blow it a couple of times to clear the mucous). I can't stress enough how this came on suddenly. By the time I finished flossing, the mucous was mostly gone, although I was still producing saliva.
I noticed this same thing, but to a lesser degree, when I downed my medication this evening (I take pills with applesauce so they don't get stuck in my throat).
I was able to consume 4 cartons of food today (still fairly long feedings - 30-50 minutes). I should be able to reduce that time. Tomorrow, because of my simulation appointment, it might be hard to increase my total, but for sure the days after that I should be able to increase it to 6. My body and stomach seem to be tolerating it well.
This morning, November 30, I coughed up phlegm (twice, this time with a little more brownish color, feels like it's deep in my throat or possibly my lungs). It's close to an exact rerun of what happened yesterday morning. Also, I had a lot of thick, sticky mucous in my nose.
And, again I woke up once last night with my skin moist from sweating.
And, my peg is still sore - not sure if this is normal 9 days out from surgery.
Temperature at 9:30 am was 97.5.
I called Banner radiology to let them know what was going on. The person I spoke with said I would be on my back for 30-60 minutes with a mouthpiece in my mouth for the simulation. I told her I couldn't guarantee I wouldn't be able to remain still and not cough for that long. She was undecided, allowing me to make the decision. I opted to cancel for today (was rescheduled for December 6).
I also called my nurse navigator and explained in full detail what's going on (left a message about 9:30 am, received a call back later, think it was around noon or so). She brought in my speech pathologist who said she would send me a technique via e-mail that might help reduce the phlegm.
I sent a photograph of the phlegm to my oncologist, Dr. Radhi.
Temperature at noon was 97.5.
12:45 pm (no more coughing since this morning).
Temperature at 2:15 pm was 98.1.
About 2:30 pm the chills started (just like last week). No coughing. The temperature in my residence is 72. I increased it to 77.
Temperature at 4:50 pm was 102.3.
Temperature at 6:00 pm was 102.6.
I reduced my residence temperature to 72 and removed my cloth hoodie.
Temperature at 7:50 pm was 100.2.
A few minutes ago I coughed up a large amount of phlegm, same color as this morning. It actually hurt my chest when I coughed it up - a lot - scary. The cough/phlegm was from very deep in my lungs.
I've been trying the speech pathologist's technique of coughing so I don't aspirate, but that just doesn't enable me to access it in one cough (I have to cough 2-3 times, then it feels like if I swallow it, per the pathologist's recommendation, It's going to get stuck in my throat).
THIS is the scariest thing I've felt and experienced so far.
It's getting more difficult to speak properly as the days go by.
It seems The Universe is just not "on board" with me.
I'm thinking it might be time to seriously think about palliative care, combined with Hospice at some point, or assisted suicide in Oregon (I think I read you need a 6-month terminal diagnosis - will verify.
Temperature at 9:10 pm was 100.9.
The month of November has been nothing short of a whirlwind for me - a "dust-devil" of the worst kind. The number of appointments I've had to keep (and all of the driving), the non-stop voice and text messages (and the countless hours responding), the endless stream of information I've had to absorb and process, insurance B.S, trying to get my will completed, the amount of money I'm shelling out - all while doing my best to not fall into an abyss of doom and gloom, and dealing with different kinds of pain.
I'm worn out. I'm tired. And I haven't even started treatments yet.
December, 2023
This morning, December 1, at 11:00 am my temperature was 97.7.
I coughed up some phlegm this morning which looked like it had a little bit of blood. Also, when I blew my nose right after, there was some red mucous.
Was able to complete my will and trust documents and have them signed and notarized today.
Temperature at 4:20 pm was 98.4.
Still coughing up phlegm (about 3 times throughout the day (still coming from somewhere deep), but all of these were that same light brownish color (no blood).
Temperature at 6:30 pm was 99.5.
Temperature at 8:00 pm was 100.9.
Temperature at 9:10 pm was 100.1.
Today, December 2, at 4:45 pm my temperature was 98.1.
No fever today, at least none I could feel throughout the day.
I coughed up some phlegm several times, but today it seemed it was coming from a different place - up higher in my throat or possibly my sinuses.
Two night sweats last night.
Today is full day 4 of only tube feeding. Just after I had figured out how to deal with constipation (from my pain medication) when eating solid food (by eating prunes, using olive oil in some of my food, and eating some whole-grain bread), now I again have constipation.
The liquid food I'm ingesting has fiber in it, but obviously not enough to offset the effect of the medication. So, realizing I needed to do something before it gets worse, I decided to try drinking a small amount of prune juice mixed with water (2 oz. of prune juice mixed with 1-2 oz. of water, twice today). I'm trying to "drink" as much water through my feeding tube as possible, and per the speech pathologist, I should drink about 1 cup of water each day to try to reduce my phlegm/saliva/mucous production.
My good friend Brandon connected me with a friend of his named Reta who is a cancer survivor. I called Reta and had a long conversation with her.
Reta had anal cancer and she is about three years out from treatment. In total, Reta did 28 radiation treatments and one chemo treatment. During her radiation treatments she quit twice, and never completed the full 35. She said she just couldn’t do any more.
Since then, Reta has been employing alternative forms of treatment (she was never pronounced "cancer-free"). In particular she is taking a very large dose of melatonin (360 mg daily).
She also let me know about a guy named Chris Wark who survived cancer and has a website entitled "Chris Beat Cancer" and a healing cancer coaching program called "Square One" .
Reta was very empathetic to my situation and it was a positive experience to connect with someone who truly understands what I'm going through.
I'm having a RAGING internal battle about which direction I should go (chemo + radiation, or some other option). I'm having a really, REALLY difficult time allowing myself to surrender to the same health care system that completely failed me in early detection, and allowing that system to just run "roughshod" over my body for at least 7 weeks.
Last night in my personal journal I noted that I've already been deprived of three of the things that bring me joy, energize me, and make me want to get out of bed in the morning: 1) working out at the gym, 2) eating and enjoying healthy food, and 3) playing the guitar (first, it would be extremely difficult and maybe impossible to play with a tube sticking of my stomach, and second, it takes energy and a certain state of consciousness to play the guitar well).
One thing that I didn't mention in my journal: the enjoyment I get from photographing Nature. Being on a feeding tube, and having a tube in my stomach (which affects my ab muscles and many of my movements), I won't even be able to day a day-trip, let alone an overnight or multi-day trip. How in God's name would I be able to feed myself? I wouldn't be able to hike up and down rocky desert areas (like the Four Peaks area, which I've been going to every spring for decades) to seek out photographs.
Add to that the Thursday chess group that has been an integral part of my life for the past seven years or so. The truth is, I have so much on my mind, and my life has been thrown into such disarray that I don’t even feel like playing chess.
Today, December 3, I felt no fever (as of 5:30 pm). The cough I've been experiencing seems nearly gone - still there a few times, but not coming from that deep place it was recently, and with little or no phlegm.
One night sweat last night.
Woke up with MAJOR constipation today - so much that it was uncomfortable to sit in a chair.
If you're squeamish, I suggest you stop reading this, right now, but it's important for me to describe this so anyone reading can fully understand what it is I'm going through.
Things were so clogged up in my rectum that I had to use a lubricated finger to actually dig out small pieces of feces, one at a time. It felt like if I had instead tried to force the feces out, I would risk tearing my anus.
I did this once, but then because my system had so much more backed up behind it, I immediately felt the need to "go" again. But, for the same reason I just mentioned, I didn't feel it was wise to attempt to force it out.
I called my cousin Linda (retired RN) to get some ideas on what I should do. After a long talk with her, I decided that a stool-softening suppository would be the best way to go. The only problem was, my feces were right there "knocking on the door" and there was no free and open space to put the suppository.
When I got back from the drug store, for a second time I used my lubricated finger to remove as much feces as possible. Unfortunately, it still felt like things were not ready to "let loose" on their own.
I decided to take a break and do a tube feeding.
For a third time I removed more feces (one small piece at a time). Then, FINALLY, it felt safe to let my body do what it needed to do. Needless to say there was a lot backed up (which was of a very firm, but in one piece, consistency, unlike the stuff I had been digging out before). Also needless to say, what a relief!
Are we having fun yet?
Today, I've increased my water intake, and will continue to do so (yes, I record all of my feedings, water intake, bowel movements, and medication intake). I'm also going to try and drink a small amount of warm (suggested by Linda) prune juice diluted with water.
Today, December 4, I was able to speak with one of Dr. Samuel's nurses (Samuels is my radiology doctor). I had called last week and asked the nurse what type of radiation treatment I would be receiving, IMRT or IMPT). She said IMRT, which was not the answer I was hoping for. I asked her to ask my doctor why I would be receiving IMRT.
IMPT is the most advanced type or radiation which, essentially, minimizes "collateral damage" to surrounding tissues and structures.
Today, I asked the nurse what she had found out, and she told me that Banner MD Anderson in the greater Phoenix area does not offer IMPT radiation treatment. She said that Mayo Clinic in Scottsdale does offer it, but she said that many health insurance companies don't cover it.
Earlier this year I called Mayo Clinic in Scottsdale. If memory serves me correct it was to find out about a particular neurologist I had been referred to. I was told that there was a 4-6 month wait to see this doctor. I was also told that my UHC Medicare Advantage insurance is not accepted at Mayo Clinic.
I did some online research (back then) and discovered that UHC Medicare Advantage used to be covered by Mayo in Scottsdale, but not any more. I also discovered that UHC Medicare Advantage IS covered by Mayo Clinic in Minnesota.
At that time I considered the option of dropping my UHC Medicare Advantage insurance and going with straight Medicare (which Mayo DOES cover), but with a wait time of 4-6 months, what good would that have done me? I needed answers right away, not 6 months in the future.
My radiology simulation is rescheduled for this Wednesday (November 6). Although my coughing and fever has fully subsided, I'm still producing lots of saliva and mucous (the same way I have been for many, many months now). I just hope that doesn't derail the simulation (you need to be still, on your back, for a long period of time for the CT scan and the actual simulation).
Today, December 5, I had an appointment with an alternate speech therapist (Ashley). I was given a set of swallowing exercises to start doing every day. I will do the exercises during my treatments to counteract the effect of radiation on muscles in the neck.
My dietician and my nurse navigator were also there for the first part of the appointment. I talked about the fact that I'm producing a fair amount of saliva and mucous, which might make it challenging tomorrow for the simulation.
It was a good meeting where lots of things were discussed. The team suggested I try Mucinex DM liquid to thin the mucous. The speech pathologist suggested I try gargling with flat ginger ale (and to bring some to the simulation tomorrow). She said that for many people it helps reduce the mucous.
As I expected, I was told that if I can't complete the simulation tomorrow, then I will start a round of induction chemotherapy by itself. That would mean two total rounds of chemo, which, obviously is not what I want to do.
I was able to express my pendulum-like, back and forth thoughts and feelings about whether or not I should, or even can accomplish the 7-week treatment plan. Ashley was very empathetic, and very knowledgeable, explaining to me some of what I might expect in my treatments over the 7-week course. I felt very good, and positive at the end of this meeting.
I weighed in at 125 lbs. which is the same as my last visit. That's an indication that the 2,130 daily calorie tube feeding is allowing me to maintain my weight.
Yesterday, thinking about what's ahead, something inside of me came to a conclusion that one way to frame this is to view it as a personal challenge, and to release (as much as possible) any expectations or concerns about the outcome. If you've been following this post, you know that I have some very good, well-thought-out, and logical reasons to just say "fuck it" and not go through the treatments (which would mean sure death at some point in the not too distant future). But, at the moment I feel really good about re-framing it and moving ahead, full-speed, with hopes that I will have a long-term positive outcome.
Today, December 6, I completed the radiation simulation. Basically, this is where you are fitted with a custom mouthpiece and a custom plastic mesh mask which covers your entire face, the sides and top of your head, and your upper torso, all of which is required for the targeted radiation treatments.
Once those have been created a CT Scan with contrast is done which I assume maps the actual cancer and structures in my mouth to the mask.
I will wear the mouthpiece and mask for all 35 treatments.
The challenge for me during the simulation (which I was highly aware of going in) was to not focus on any phlegm that might form in my throat (the same place where it's been collecting for many, many months now). Even though I blew my nose (lots of mucous there lately), coughed, and cleared my throat and mouth completely before lying down for the procedure, 5-10 minutes into I could feel some phlegm collecting.
It's a very annoying feeling, you really want to get rid of it by coughing it up and spitting it out, and you just hope it doesn't try to make its way down your throat so you are forced to cough (you must remain absolutely still for the procedure). At one point I felt I just had to clear it, but by forcing myself to think of other, more pleasant things, I was able to make it through.
What's interesting to me is that even though immediately after the procedure I asked for something to spit into, it wasn't until I got back to my vehicle that I was able to finally cough up and spit out the phlegm that collected during the procedure (it takes a certain type of cough, done multiple times to bring it up).
Seeing my feeding tube, the nurse that prepped me today asked me if I ever felt hungry. What's strange is that I haven't even thought about, or felt hunger, not even once, since I started tube feeding exactly one week ago. I wonder if that will change over time?
I was given a lot of paper handouts regarding radiation. The side effects, both short-term and long-term, are extensive. I was already made aware of most of these in my initial MDC meeting when I spoke with my radiologist Dr. Samuels. Reading through the handouts makes pause and think, what if I did just chemo and passed on the radiation? If I was receiving IMPT radiation I wouldn't be as concerned, but with IMRT (more "collateral damage") it really makes me wonder. I'm assuming my medical team wants me to do both because they think that will give me the best possible outcome.
My first radiation treatment is scheduled for December 19. From what I was told yesterday, my first chemo treatment will be scheduled on that day or shortly thereafter.
Reta, the cancer survivor I spoke with a few days ago, connected me with a friend of hers named Eric who is also a cancer survivor. I called Eric, and despite the fact that he was still recovering from two recent heart attacks, he shared his story with me.
In 2011 Eric was diagnosed with squamous cell carcinoma at the base of his tongue (same as mine). Unlike me, he didn't have dysphagia. Once the cancer was discovered, Eric had it surgically removed within 10 days. Eric wasn't given a cancer stage number, and he had no chemo or radiation. As a result of the surgery, he lost the bottom salivary glands in his mouth and the surgeon removed all surrounding lymph nodes.
If you've been following this post, you may recall that the first doctor I saw was a head and neck surgeon. She ruled out surgery. She said it would be too destructive and have too great an impact on the quality of my life. If my situation had been diagnosed sooner, it's possible that surgery would have been an option.
Today, December 7, I got the full schedule for December 19. I arrive at 8:30 am for lab/blood work. First radiation treatment at 9:40 am. Meeting with oncology nurse at 10:30 am to discuss my chemotherapy treatments, after which I will have my first treatment (could take 3-4 hours).
I was told by the oncology nurse today that I will be able to drive myself home afterwards. She said the first and second days are fairly easy, but the third day is when I might feel some side effects (will get more info on Dec 19).
Finally, today I emptied out and cleaned my refrigerator. The refrigerator was a mess (hadn't been cleaned in ages) and there were a few things going bad, but now it's both nearly empty and very clean. I never in my life thought that one day my refrigerator would look like this:

Today, December 8, for the first time in a really long time I actually felt a sense of calm. I had almost forgot what calm felt like.
My traMADol pain pill got stuck in my throat this morning. Without it I would have a constant headache and it would be really hard to function.
I called my nurse navigator at Banner to see if they have a liquid version I could administer through my feeding tube. She said that because the traMADol I'm taking is immediate-release (not time-release) I can simply crush it, add some water to dissolve it, then administer it via my feeding tube.
Good news regarding bowel movements. Since the major constipation I experienced back on December 3, I'm happy to report that things seem to be back to normal. I attribute that to a significant increase in my daily water intake along with a small amount of diluted prune juice.
I'm still having night sweats (usually twice each night).
Today, December 9, the excessive mucous and saliva (phlegm) continues. It seems like it's gotten a little worse over the past several days. When I say excessive, I mean as soon as I spit out a mouthful of it, in less than one minute I have another mouthful to spit out. Sometimes throughout the day it seems to be almost constant, and at other times not so much. I keep an empty glass available at all times, wherever I am, so I can spit when I need to.
I've discovered a certain way of coughing that usually brings up a large amount of phlegm (seems to collect in the back of my throat, where my sinuses empty into my throat).
Brushing my teeth at night always generates a lot of phlegm.
Today, December 11, I had my first appointment with my new PCP, Dr. Kirsten Knobbe Lloyd, MD at Archwell Health (weight 123 lbs.). Archwell Health focuses on senior care. Dr. Knobbe was cordial, thorough, professional, and spent alot of time with me (my appointment lasted at least 45 minutes).
I started taking 5 ml doses of Guaifenesen (liquid) every 4 hours to loosen mucous.
Today, December 12, I completed a hearing test at the request of my team at Banner MD Anderson. The reason for the test is to establish a baseline against which they can compare after my cancer treatments (particularly the radiation).
Today, December 13, after doing some online research into how to prepare your living environment for chemotherapy, I decided I must move all of my house plants (18 in total) to my screened-in patio. The soil in houseplants can house tiny bugs (which I often treat for), mold, and other things that could potentially be a problem for me when I'm in an immuno-compromised state. Hopefully, we don't have any really cold weather over the next couple of months. This also means that watering will be much different than usual. Instead of placing each plant into my kitchen sink and watering until water runs out the bottom of the container (the correct way to water houseplants), I will have to give them much smaller amounts - just enough to keep them alive.
I purchased and installed one of those allergen air filters to replace the cheap ones we get from the office where I live. Filtering out as much dust and pollen from the air is a requirement.
Bathroom hand towels and kitchen dish towels are out, replaced by paper towels. The kitchen sponge I used to use to clean up around the sink - in the trash, replaced by Lysol disinfectant and paper towels.
I also purchased some sanitized wipes to use on door knobs, the steering wheel of my vehicle, and anything else I often touch.
I've been wearing a mask whenever I'm in close contact with people (which isn't all that much) and I will continue to do so throughout my treatments.
I've been cleaning a lot over the past few days, and that will continue through the weekend until things are as clean as possible.
Bowel movements are just barely OK. Even though I've increased my water intake significantly, things are just barely getting by down there. I'm going to try and increase my intake of prune juice as well.
I received a call today from the person who will be doing my radiation treatments. She said the treatments should take 15-20 minutes, and that they would all be scheduled for early morning (9am - 10am). That time frame is the best time for me in terms of least mucous and saliva (the hour or so right afer I get up).
I have an appointment to meet with my speech pathologist on December 15 (this Friday). In my last meeting with speech pathology (December 5) I was given a list of swallowing exercises to do 4 times each day. I've been doing a reasonably good job doing them, and they will become more important I'm sure as I begin radiation treatments (radiation, I was told, tends to stiffen your muscles).
It's become more and more difficult to speak properly (because some of the cancer is at the base of my tongue, it's affecting my ability to speak).
The only thing I've been taking by mouth (now that I'm crushing pills and dissolving them in water) is a small amount of water throughout the day. Everything else is via my feeding tube.
Today, December 14, more cleaning (dusting and vacumming indoors), and I did a major cleanup of my screened-in patio. For those of you who don't live in the deserts of Arizona, it's a very, very dusty place. Add to that dust storms in the summer months, and after a full year a screened-in patio like mine is just thick with dust and leaves (which blow in through the bottom of the security door). So, wearing an N95 mask (and being very careful to not stir up too much dust) I tackled that dirty job, removing all the screens, hosing them down, sweeping and vacumming the patio floor (indoor/outdoor carpeting), then transferring all of my houseplants to a clean patio.
Today, December 15, I had another appointment with my speech pathologist Leah. In addition to reviewing the swallowing exercises I was given on December 5 (which I have been doing several times each day), Leah and I reviewed the MBS Test I had done on November 17. Leah said the study showed I was not aspirating at all with liquids (water) as long as I take smaller sips and don't try to swallow multiple times in quick succession (gulping). She said I should increase my water by mouth intake to two cups per day.
Leah watched as I swallowed small sips of water. She commented that my larynx seems to be elevating more compared to what was shown on the MBS Test. She said that's a good thing, and it shows that perhaps the swallowing exercises are working.
Laryngeal elevation is a key issue for me because it helps prevent aspiration.
When she had me try a small amount of applesauce I was able to swallow it, but even after swallowing four times it felt like not all of the applesauce had cleared my throat. Leah said that this pooling has nothing to do with my cancer, but most likely a problem with my upper esophageal sphincter (UES), also known as the cricopharyngeus muscle. The UES relaxes and opens during swallowing, then shuts tight after swallowing to prevent the reflux of foods from the esophagus into the throat. With me, my UES is always tight, which creates the pooling, and the feeling that you have to constantly clear your throat.
She also said that my epiglottis (the lid which covers your larynx to keep liquids and food from entering your trachea/windpipe when you swallow) is not functioning properly.
The bottom line for me to address these issues is to continue to do the swallowing exercises, especially the Shaker exercise and the Mendelsohn exercise, both of which help with laryngeal elevation.
Because I'm still losing weight (weight today was 123 lbs.), Leah sent a message to my dietician to see if my food intake should be increased.
On December 16, around 7:45 pm, I was unable to pass a bowel movement (the previous day I had a moderate-sized movement that was chunky and somewhat difficult). Once again I resorted to a gloved, lubricated finger to try and remove some of the chunky stool. I was successful to a degree, but the stool was too large to pass.
I had this intense feeling of needing to go, but I was unable.
I texted my cousin Linda. Despite our conversation and her advice, it got to the point around 8:30 pm or so that I decided to go to HonorHealth ER. The feeling was horrible, and I was almost panicking.
The wait at the ER was 2-2.5 hours. While waiting I paced back and forth (sitting was very uncomfortable). I also made at least three trips to the men's room while waiting, at one point using my bare finger to try and help things out, but to no avail. By this time my backside was an absolute mess.
Finally, I was admitted. After a conversation with me, a nurse said I needed an enema. Another nurse prepared the enema. One of the ingredients was hydrogen peroxide. I asked her if that was going to sting or cause pain and she said no.
I got the impression that this nurse had not done an enema, or had done only a few.
When she attempted it, I felt a horrible burning sensation in and around my anus, so much so that I involuntarily pulled away, screaming with a burning pain.
The nurse immediately stopped and said they would try something else. As it turns out, I think some of the fluid did make it up into my rectum.
Plan B was to get a CT Scan of my midsection to make sure there were no blockages (physical or impacted stool).
By this time it's around midnight or so. I waited about two hours to get the CT Scan. The nurse had failed to give me the call device and I became very, very cold. At one point I felt I had to try and have a bowel movement. I began calling out, hoping someone would hear me. Eventually a nurse came and I was finally able to pass some stool (yes, it was a relief) and get extra blankets (why is it alwyas so damn cold in hospitals?).
My backside was ahuge mess and it took me quite some time to do a major cleanup back there, employing several washcloths, warm water, and soap.
By now it's 3:30 am or so. I haven't have anything to "eat" since 7:00 pm or so the previous day.
Because they administered a bag of fluids (via IV) my water intake was OK. However, I was coughing and spitting up thick, sticky mucous the whole time while waiting for the CT Scan (I hadn't had any of the liquid guaifenesen I've been taking every 4 hours to loosen the mucous).
The CT Scan showed no blockages. When I pressed the nurse to see if impacted stool is considered a "blockage," he consulted with the doctoe, came back and said yes. He said that doesn't mean I might still have hard stool, but that it was passable.
They prescribed (even though it's over-the-counter) Miralax (polyethylene glycol) and called it into my pharmacy for later pickup.
Shortly therafter I was released. When I got into my vehicle the time was 5:20 am.
I showered, from the waist down, making sure to thoroughly clean (again) my backside (if you've never had a boil on your backside, often from feces, the consider yourself lucky).
It was at least 6:30 am when I finally crawled into bed.
Today, December 17, I had a small bowel movement (chunky) and felt some distinct irritation when defecating (I'm sure this ordeal tore at least some tissue back there).
I picked up the Miralax. I asked the pharmacist if there were any drug interactions with the three things I'm taking - he said no.
For starters, I tried just a little less than the recommended dosage (to see how it affects me), making sure to mix the powder until fully dissolved, then administering it via my feeding tube. In total (Miralax mix and additional water) I took in 5 ounces (3 ounces Miralax solution and 2 ounces of additonal water).
I haven't had a pain pill since yesterday morning (skipped my dose last night because I was at ER). It's interesting that so far I haven't felt much head pain. Honestly, I'm afraid to take it for fear of a repeat of what I just experienced, although I know I will need pain meds at some point soon.
I noticed a big increase in phlegm today.
Today, December 18, still no bowel movement. I took another dose of Miralax.
I contacted my nurse navigator to let her know what transpired with my ER visit, and to ask a few other questions.
Regarding the constipation, she said take a second dose of Miralax later in the day (evening) if things are loosening up. She also told me to speak with Dr. Radhi tomorrow about a stool softener like Peri-Colace.
Regarding the increase in phlegm, she said it's probably because I stopped taking traMADol. She said to start taking it again (I took one this morning) and that we will have to address the constipation side effects of that with other meds (like Miralax and others). It's important to reduce phlegm so I'm able to get through the radiation treatments and so I'm not coughing it up all the time.
Yesterday, without the traMADol I noticed some head pain, but it was tolerable. Today, the pain was worse and it took a couple of hours for the medicine to take effect. I think it would be very difficult to function without the pain medicine.
Regarding the Guaifenesin, she said yes, OK to increase to 10 ml per dose.
By mid-afternoon I was very constipated, again. It was feeling a bit like what had happened two days ago.
I contacted my nurse navigator. She said to try a solution of Phillips' Milk of Magnesia (30 ml) and 4 oz. of prune juice, warmed, diluted with water, one time. She said that for sure would get things moving. If not, she said to take another dose of Miralax at bedtime. Her concern, and mine, was that I would end up with diarrhea - not good considering tomorrow is my first day of treatments and it's going to be a very long day.
I was getting panicky, again. As I was leaving to go to the drug store I felt the urge to go, sat down one last time and was able, with difficulty, to pass a fairly large, hard stool.
Getting back from the drug store I prepared and took the solution. About 30-45 minutes later I started having watery bowel movements similar to diarrhea. For the rest of the day I had a bunch of watery bowel movements mixed with small pieces of stool. I'm hoping this will be over by morning.
My nurse navigator told me to ask Dr. Radhi tomorrow about getting me on a daily stool softener and laxative (like Peri-Colace).
I also contacted my dietician, Anne, to let her know I'm losing weight (down to 123 lbs. despite that fact that I'm consuming a full 6 bottles of nourishment each day). She said to increase it to 7 bottles, and to increase my water intake by 300 ml to help deal with constipation.
I didn't mention this to her (didn't think of it), but I think the fact that I haven't been to the gym in about 4 weeks is part of the reason I'm losing weight (losing muscle mass). Going to the gym has been problematic because a) my energy level hasn't been that great overall, b) being in an enclosed area with other people is risky for me (chance of picking up an infection), and c) I would be very limited in what I could do anyway because of the feeding tube in my stomach.
Did another trip to Costco today to stock up (even more) on bath tissue, Kleenex, and paper towels.
December 19, Treatment Day 1
Weight: 122.6 lbs. (with shoes off)
Long day today. I left home at 7:30 am, got back at 5:30 pm. Tuesdays are my radiation and chemo days.
Protocol for today (and all Tuesdays) is 8:30 am labs/blood work, 9:40 am radiation treatment, 10:30 am meeting/check-in with chemotherapy team, noon - 5 pm infusion (with some times becoming earlier as the weeks progress).
I feel a little soreness in my throat. I assume this is from the radiation treatment.
The radiation treatment in total took about 15 minutes: 5 minutes for the techs to get me properly aligned on the hard, narrow table and to affix the mask over my head and upper torso, and about 10 minutes for the actual treatment. I did not have a problem with phlegm and pooling. In fact, my mouth was relatively dry (which is hard to understand because all morning long prior to the treatment I was spitting saliva and mucous into a cup).
In the meeting with my chemo team I talked at length with Dr. Radhi's Nurse Practitioner. Monica, and the Banner pharmacy lead Donna. After a long discussion, we agreed I should try the Miralax once each day, taken late in the evening. If I go another day without a bowel movement, I should then do another "Brown Cow" (as the nurses call it) - that mix of Phillips' Milk of Magnesia and prune juice. This is still work in progress, and it might change again as I start chemo because chemo can cause constipation or diarrhea.
If I have nausea, I was told to take one Ondansetran (Zofran) 4 mg under the tongue, and if necessary another one, one hour later (one 8mg dose every 4 hours).
I was told that the dosage of chemo I'm receiving is somewhat less than what I would get if I did just chemo alone (this lower dose is customized to my body to work with the radiation).
I was told, again, that the 3-4 week point is where things start to get a little "dicey" with more pain and dehydration. This will probably mean increasing my traMADol or changing to something stronger (which would have increased side effects).
I was also told to pay attention to fever, chills, and night sweats. If I have any of these and I have a fever of 100.4 or greater I was told to go immediately to ER, tell them I'm having chemotherapy and a fever so they will give me an IV with antibiotics.
I was given a lot of literature on chemotherapy, including a phone number that goes directly to the chemo nurses.
When I asked what I should do if I get to the point where I can't speak properly enough to leave an intelligible message, I was told that messaging via the Banner portal (which I'm on) are checked throughout the day.
I was also given a printout of my entire 7-week treatment schedule (including all treatments and appointments).
My actual chemo treatment was late getting started (around 1:00 pm).
First, I was given two infusions of anti-nausea medication (Fosaprepitant (Emend) 150 mg and Ondansetran (Zofran) 16 mg) and one infusion of a steroid (Dexomethasone (Decadron 12 mg)). I was told that one of the anti-nausea medications should last up to 72 hours. This took about 1.5 hours.
Second, I was given a large bag of cisplatin - the chemo drug. This took about 2 hours.
Third, I was given 500 mg of hydration (basically saltwater) to make up for the water I wasn't able to intake because of being in therapy all day.
Tonight, I'm feeling decent considering I'm still behind on sleep (I will catch up tonight). Also, because I was up so early this morning to take my pain med, my head is hurting again (my schedule today threw my usual med schedule off). I am feeling some dryness in my mouth - need even more water.
And, with the start of radiation, tonight I started my new nightly tooth protection regimen which includes (after flossing and brushing with a prescription toothpaste) rinsing with a baking soda and water solution, 10 minutes of tooth trays with flouride, followed by keeping the leftover flouride in your mouth for 30 minutes after you take the trays out.
December 20, Treatment Day 2
I had my second radiation treatment today. I was thinking that anyone with claustrophobia might have a real problem having a mask/mesh/cage locked down over their head and upper torso for 10-15 minutes while having a rather large mouthpiece in their mouth. I think I noticed it more today because for some reason I'm having a bit more head pain today, which made "wearing" the mask somewhat more uncomfortable.
More constipation issues today. I did not have a real bowel movement yesterday (last one was the day before) - just the aftermath of the "Brown Cow." I did another "Brown Cow" today which produced a lot of diarrhea (similar to two days ago) all afternoon and into the early evening, but still waiting for something more major to move.
I communicated this information to Monica (Dr. Radhi's Nurse Practitioner) and received a very short response from one of the other members of her group which seems to be saying that I should stay with this protocol for a while (that's my interpretation of their response).
Obviously, with this much diarrhea I had to increase my water intake significantly today, and it seems that will have to continue for at least the immediate future. That means my afternoons and early evenings will be centered around my toilet. It might even make going for a walk out of the question - not good.
The large volumes of phlegm continue, almost continuously much of the time. I have a "spit cup" and tissue at hand nearly all the time.
December 21, Treatment Day 3
Weight: 125.5 lbs.
Today I had my third radiation treatment followed by an appointment with my radiology doctor, Dr. Samuels.
He suggested I try Acetaminophen for my headache.
When I asked him about the potential increased pain in my mouth (and possible mouth sores) as the radiation treatments progress, he said the remedy is increasing or changing my pain medication (he said I might need to take Percocet).
He confirmed that the radiation I am receiving is targeting not only the base of my tongue but the two growths near my lymph nodes (left and right).
Regarding the effect on my salivary glands (they stop producing, which is also bad for the teeth), he said that effect is usually not permanent.
Regarding the dental trays with flouride, he said that starts three months AFTER my treatments. I was under the impression I should do that during my treatments.
Regarding constipation, he said it's OK to take Miralax twice a day.
His nurse practitioner, Teri, said I should use a moisturizer on my neck (store bought) where I'm receiving the radiation. Later during treatments she said I should use Aquaphor.
Also, I received a call from my new PCP's office at Archwell Health, inquiring about my ER visit last weekend. I was able to have a discussion with my new PCP, Dr. Knobbe. I explained to her what's been going on with my constipation. She said that she's treated patients before using Miralax multiple times per day until it produces a bowel movement or diarrhea, and that you can't overdose on it. The trick, she said is finding an amount (dosage) that works, and that might mean multiple times per day.
She also said that Archwell has people on call 24/7 and on holidays that I can call if I'm having some medical issue and I need advice on what to do.
I did another dose of Miralax this afternoon. A couple of hours later I finally did have a bowel movement (fairly loose, but at least things are moving).
Tonight, I've been feeling a bit of a sick feeling, off and on, probably the result of the chemo.
My phrase for today was "SLOW DOWN" in everything I do. Slow down and be in the present moment. What I'm going through can (and often does) consume you, as I've already experienced. My challenge, which I'm working on, is to not let that happen, or at least minimize it. As things get more challenging that might become more difficult.
Had a nice long walk today in 75-degree, sunny weather, just enjoying the feeling of the sun on my skin and everything else around me.
December 22, Treatment Day 4
Woke up before my alarm clock was set to go off. Wasn't too long afterwards that I started to feel sick. I seem to remember just sitting on my couch for a while, hoping the sickness would pass. A while laterI got up and decided to take my morning meds - was able to get that done. Then, I got really, really sick - that feeling where you have to sit down as it washes over you like a wave.
Then, I started to sweat, all over. I removed my hooded, cotton top, put my arms down on the table and rested my head on them as the sickness continued. At one point it felt like I might even pass out.
After that feeling peaked, I still felt really sick, certainly in no condition to go to therapy. I had already set up the possiblity of a driver (my friend Diane) for today, but because I'm prone to motion sickness (have been all my life), being a passenger for a 25-minute drive (probably much longer because it's raining in Phoenix today) would probably only make me feel worse and possibly vomit.
I called Teri, the radiation nurse and let her know how I was feeling, and that I would not be able to make it today.
I told her I didn't think I would be able to take the nausea medication via mouth (sub-lingual) and I asked her if I could crush it - she said yes.
I did that after hanging up the phone - it seemed to help some, although it's hard to say for sure (could have been that the sickness just passed on its own).
After intaking some water, I just sat on the couch, closed my eyes and rested. I had told Teri that it felt like my body just needed to rest. So that'w what I did.
Some time later I got up and decided to try one bottle of food (my usual dose is 1.5) - was able to get that done.
More rest.
Later, around noon, I did another dose of Miralax.
Will spend the rest of the day resting, nursing my food down slowly, and most likely taking at least one more dose of Miralax (which I took later in the day).
My body does not deal well with any kind of nausea (never has). I was dreading this possibility (from the chemo I assume, since today is 3 days out).
This, in total, is the most unpleasant, horrific thing I have ever in my life experienced.
Today, December 23, I spent another day trying to figure out the best dosage of Miralax. I took one dose earlier in the day, had a somewhat loose bowel movement later, then a very loose, diarrhea-like movement later on - not what I want to happen.
Also, I still have that headache that started a couple of days ago (mostly on the right) - not sure what that's about. I've been taking Acetaminophen which seems to help some. Yes, I could increase my traMADol to three times per day, but then I introduce the possiblitily of more constipation, which, after what I've been through already I really, really don't want to do unless I have no choice.
I took a long hot shower tonight which felt really, really good. It seemed to calm the mucous in my throat for a while after as well.
Today, December 24, Christmas Eve, I woke up and when I coughed up a big wad of phlegm from the back of my throat there was blood - more than I've seen before. Yes, this concerned me, but rather than call the triage nurse at Banner (they would probably just tell me to go to ER) I e-mailed my cousin Linda to get her take on it. She said it's normal for pharyngeal cancer patients like me to experience this. She sent me a link which discusses something called Mucositis. It sounds pretty serious. This is something I will definitely be mentioning to my team on the 26th.
Bowel movements are very, very small (had a couple).
Headache still persists on right mostly.
Today, December 25, Christmas day, I had a nice long walk in 60-degree weather with full sun. It felt really good.
Constipation still an ongoing issue.
December 26, Treatment Day 5
Weight 119.6 lbs.
Today was my long day. I got up and was on the road by 6:30 am (pre-sunrise, 46-degrees, no heat in my vehicle). I didn't get home until 6:30 pm (post sunset).
Today I had my fourth radiation treatment (labs/blood work prior at 7 am), a meeting with my chemo doctor, Dr. Rahdi, then infusion (chemo).
Because of the time between those events, and because my infusion was 75 minutes late getting started - that (along with driving time to and from) accounts for the 12-hour day.
I talked about ongoing constipation issues with Dr. Radhi. She said to add one Senna-S tablet to my daily Miralax regimen, and to increase the Senna-S if necessary.
I also mentioned the blood I coughed in my phlegm recently. I mentioned Mucositis - she didn't have any response to that specifically, but she did express concern with the bleeding and confirmed that yes, the lining of my throat is affected (skin cells are destroyed, making the lining thin in places) by radiation.
Dr. Radhi also reviewd my blood work. She said that of the two white-blood cell markers one is good, and the other just a little below what it should be (3.4 instead of 4, but that it wasn't enough to adjust my cisplatin).
I haven't had a normal bowel movement in several weeks. I can't begin to tell you much of a pain this is. According to my cousin Linda, my bowel movements might not get back to normal until my treatments are over and done with. At the rate this is going, I might need diapers.
Didn't have my first "meal" until around 7:30 pm, but before that, the first thing I did was take my daily Miralax.
The plan for this coming Thursday and Friday is to start taking Zofran (newly prescribed, 8 mg pills) on Thursday later in the day, then take another during the night (maybe 4 am) in hopes of not getting too sick so I can make it to my Friday radiation treatment.
As I said to my cousin Linda on the phone tonight:
This is fucking INSANITY!
December 27, Treatment Day 6
Still dealing with constipation. Today, for the first time in several days I did have a small bowel movement (3 small pieces, oblong, about 2-2.5 inches in length).
What started happening as of yesterday is that I get a small amount of leakage down there, throughout the day. It almost feels like the normal contractions in my bowels have shut down.
Needless to say this is a messy situation, and not my idea of a good time.
I've been applying Aquaphor ointment to that area for a number of days now to help it heal, but when I clean that area before applying it, it might take 4-5 wipes of the washcloth because of the leakage.
I started taking the Senna-S today, and will continue once a day for a few more days to see if it helps. It is designed to help soften stool and stimulate bowel muscle contractions.
I discussed all of this with my cousin Linda last night and she said it's all normal for cancer patients.
Regarding weight loss, I've been exchanging e-mails with my dietician Ann. Today I increased my daily intake of nutrition from 6 cartons per day to 7 per day (that's an additional 355 calories per day).
Also today, I had a few shorts rounds of hiccups. After doing a little research, it looks like this is a side effect of the cisplatin chemo drug I'm being given.
And the phlegm just keeps on coming. I carry a cup with me wherever I go (at home, grocery store, at Banner) so I have somewhere to spit. It's almost constant throughout the day. As soon as I spit some out, there's more to spit. In addition to that (as I've mentioned before), at least once an hour (sometimes more) I cough up much larger wads of phlegm form deep in my throat - so large sometimes that it almost makes me gag. It's disgusting, but I have to get that stuff out.
I paid a bunch of medical bills today. My total out-of-pocket just went over $2,000.00.
December 28, Treatment Day 7
Weight 124.6 lbs.
Today was a VERY challenging day. I finally had some bowel movements, but they came in rapid succession four times over a 5-hour period (mid-afternoon into the evening). Unfortunately, the third one ended up in my underwear. You know that sticky poop that young infants produce? Yeah, we're taking that.
Needless to say I had a royal mess to deal with for about 5 hours, and each "clean up" took a very long time as stuff kept leaking out. After the third movement it was time to surrender and get some Depends (well, not actually Depends, but the Kroger brand).
The takeaway is that it's time to backoff of the Miralax and just go with just the Senna-S for a day or two and see what happens.
There is a delicate balance between diarrhea, too much sticky poop, and constipation.
I've been craving real food, in particular the Chicken and Broccolli from the Saigon Bowl restaurant right around the corner (which I drive by often).
December 29, Treatment Day 8
Last Friday I was not able to make it to my radiation treatment because I felt so sick (from the chemo). Today, I was able to make it. I took a Zofran (for nausea) last night around 8:00 pm and another one around 4:00 am this morning. Not sure if that was the difference from a week ago, but that's what I will do going forward.
Friday's are going to be my "feeling a little sick" day it seems (third day after chemo). My enerrgy level was less today, but I did get out for a nice walk. I actually laid down and slept for a while this afternoon. I had a dream that I was eating real food, and yes, it was indescribably delicious!
I hope and pray that after my treatments I will, at some point, be able to eat and enjoy real food again. It's hard to put into words how much I miss that simple pleasure in life.
Today, I had just one bowel movement (similar to those from yesterday afternoon).
December 30
About a month ago I had a conversation with a neighbor of mine named Shannon. I told her I had cancer. In our conversation I told her that most likely my cancer was caused by HPV. I also told her that the REAL, ROOT problem is why my body was not able to ward off the HPV.
To that end, I will be closely examining my thoughts, my emotions, and all other aspects of my life to determine what I need to change moving forward.
I already know some of what needs to change, and with this cancer "wake up call" I will make those changes immediately.
Other things might take more time to ascertain.
December 31
Those of you who know me know that I have been tracking and documenting the "trials and tribulations" of a certain American political figure for the past eight years on my Health and Wellness Resource website (not going to say his name, but you know who I'm talking about).
During that time I felt obligated to do so because that person posed, and still poses a huge threat to American democracy.
The person of whom I speak is, by far, one of the most vile, reprehensible, egotistical people on planet Earth.
Therefore, effective immediately, I am letting go of this individual and everything he represents. I will no longer track, document, or comment on him moving forward. I will read only headlines, and listen to whatever is reported on the PBS Newshour and NPR. Nothing more.
My personal health and wellness is far, FAR more important.
As my friend Brandon said last night, this person "feeds on hate." Hate and negativity are toxic to all humans. That's especially true for me right now.
January 1
Had a small bowel movement today but certainly not back to normal. No constipation, but I need to stay vigilant and continue to pay close attention and modify my laxative intake accordingly.
January 2, Treatment Day 9
Weight 120.6 lbs.
Not quite as long a day today (on the road at 6:30 am, back home at 4:15 pm) as my infusion treatments for the next few weeks are scheduled for 11:00 am instead of 1:30 pm.
White blood cell markers are holding steady.
I did not feel the need to take a pain pill last night (no head pain), so I didn't. I did take one this morning.
January 3, Treatment Day 10
The big news of the day is that I FINALLY had a normal bowel movement. This is the first normal bowel movement I've had since the first week of December (yes, I keep a daily log). I never in my life thought I would get so excited about something like this! As a result, I was able to relinquish the use of my "designer underwear."
January 4, Treatment Day 11
Weight 125.4 lbs.
I feel like I'm trapped in a time warp. Some alternate state of reality.
I am SO sick of having my kitchen looking so foreign and unappealing - a place where I "administer" what's necessary to survive.
I want my life back, the way it was before all of this started.
January 5, Treatment Day 12
Nothing of consequence to report.
January 6
The flow of saliva and mucous in my mouth and throat is nearly non-stop. What's worse is that at least twice an hour I cough up a large wad of phlegm from deep in my throat. When I do that if makes me feel like I'm gagging. To say it's disgusting doesn't even come close.
The phlegm is slightly irritating. I tested it with PH strips and it's coming in a little less than 6.0 (7.0 is neutral) which is acidic (not good for teeth and gums).
To deal with it I've now been rinsing my mouth out with water every time I spit.
Also, I purchased an alkaline water pitcher which is producing water at a PH value of around 8.0. I now use that water to rinse hoping it will help neutralize the acidity.
January 8, Treatment Day 13
Weight 121.1 lbs.
January 9, Treatment Day 14
Weight 121.7 lbs.
According to Dr. Radhi, white blood cell markers are slightly down from last week but not enough to postpone treatment.
Something new has cropped up. I've been having numbness in the bottom of my feet and some in my legs from time to time. This is someting I addressed with physical therapy earlier this year, but over the past 2-3 weeks it's been getting more noticeable. I did some online research and discovered that neuropathy is a common side effect of some chemotherapy drugs drugs, including cisplatin.
I discussed this with Dr. Radhi today. She confirmed the research I did. She said it's a balancing between administering enough chemo drug to kill all the cancer, but not giving so much that it causes neuropathy (or at least mimimizes the effects). After I described my symptoms to her, going back to earlier this year, she said she would descrease my cisplatin dosage by 25%.
Today, I decided it's time to start doing some home resistance exercises (similar to the program I did during COVID when gyms were closed). I need to make a concerted effort to make this happen, and to slowly (if possible) increase my physical fitness activity, which until now, just wasn't feasible due to the myriad of things I've been dealing with.
January 10, Treatment Day 15
Unfortunately, today I went down another LONG, DEEP, and WINDING insurance/billing rabbit hole. All I wanted to know was how much the formula and supplies are going to cost me (to date I haven't received any bills, which seems odd). That's it. Sounds like a simple, straightforward question, right?
Maybe in Canada, or the United Kingdom this question wouldn't even need to be asked because I would know up front. But in the good old USA, nope.
I won't go through all of the "gory" details. Suffice it to say that I talked to at least four different people (one from United Health Care, one from Optumcare Arizona, and two from another entity I was referred to by Optumcare called Optum Rx) and spent about two hours on the phone. It turns out that Optum Rx is actually called Optum Special Pharmacy and has absolutely no association or affiliaton with Optumcare Arizona. Why would I have been transferred there?
I pleaded my case to the UHC support rep and told her it wasn't my job to make all of these phone calls (when she said I needed to call the forumla supplier). I had already gone to great lengths trying to get information from them over the past three weeks but they would not respond to my inquiries.
I turns out that a prior authorization was just recently processed by Optumcare Arizona. So, in a few days I will try, once again, to call the formula supplier becasue by then they should know how the billing will break down (I was told by UHC today that my co-pay is 20%).
I could scream!
I saw the other speech pathologist today, Ashley. She's really on the ball, very empathetic, and a wealth of information. She thinks I'm doing really well and encouraged me to keep doing what I'm doing. She also confirmed that the next couple of weeks might be more difficult regarding the effects of radiation, but she also said that I might be one of the lucky ones who don't get really bad side effects. Time will tell.
Regarding when I might be able to try real food, it sounds like that's going to be a while. She said I will need about two months for my body to recover and heal from the radiation treatments before we can conduct another swallow test (need that to see if and how much I'm still aspirating). That would put the swallow test into early April. But, she said that depending on how things go I might be able to try small amounts of "easy" food before that. Of course, nothing is being said about how my swallowing or speech will be when all treatments are done because no one can say for sure.
She did say that the pooling in my throat might require a dilation of my upper esophagus. That would also have to wait for two months after treatment is completed.
One more thing to report. Tonight I noticed that there was a bit more hair in my comb when I combed it out after taking a shower. I hope that's not a harbinger of things to come, but I know that hair loss is a distinct possibility.
January 11, Treatment Day 16
Weight 125.5 lbs.
Today I spoke with a long-term friend of mine named Dave. I've known Dave since the mid-1980's. He was the realtor that helped me find and purchase a home, which I lived in for about 12 years. Dave and I also played a lot of Mesa city league basketball in our thirties, along with a couple of other guys.
Dave told me that he had just brought his wife home from outpatient surgery to fix two bulging discs in her neck. As we talked, I asked Dave what his wife's symptoms were, and how long they had been going on. Dave told me that it took doctors three years to finally figure out what was wrong with her. THREE YEARS! He said doctors seemed to leaning in the direction of multiple sclerosis for some time, but they couldn't put their finger on it.
It wasn't until a doctor suggested they do some imaging of his wife's neck that the root cause became apparent.
Dave and I both agreed that there is something terribly wrong with our health care system when it takes that long to discover something that was so easily found with simple imaging.
If you've been following my saga you know that it was an MRI and a follow up CT Scan that finally shed light on what was really going on with me.
I've already expressed my opinions about our health care system but I'll say it again. I'm not going to candy-coat it - it sucks. There's no way it should have taken the better part of a year to discover I had cancer, and there's no way it should have taken three years for Dave's wife to find out she had bulging discs in her neck.
The problem, in my opinion, based on my recent experience with many different doctors, is that doctors just can't seemed to think "outside the box," and that they can't seem to just step back and look at things from a higher, systemic, body-wide level They all seem to be locked inside of their own little spheres of knowledge. And those spheres, in my opinion, seem limited to medically-oriented procedures that they routinely do. And, the different doctors (in my case a PCP, a Gastroenterolosigt, an ENT, and a Neurologist) don't commmunicate with each other.
January 12, Treatment Day 17
Nothing of consequence to report.
January 13
The good news is that I seem to have my bowel movements under control, for now.
The not-so-good news is that I continue to shed hair when I comb it out. This morning I actually thought that maybe the best thing to do is just have it cut really short (so I don't have long, shedding strands of hair to deal with). I'm guessing it won't be too long before I'm bald. Just something else to look forward to.
January 15, Treatment Day 18
I had to cancel my radiation appointment for today due to nasal congestion.
Last night, after blowing my nose my left nostril started to bleed - not profusely, but more than I've seen happen recently. I did one of my "head with towel over basin of hot water" to try and get some humidity in my sinsues which seemed to loosen things up, but there was still blood in my left nostril (and I was seeing it he phlegm I was coughing up.
I had asked Dr. Samuels about blood in my nostrils last Thursday. He said it was due to the dry winter air and not cancer.
This morning I woke up very, very congested (some in right nostril as well, but mostly the left) and having difficult breathing through my nose at all (along with more blood in phlegm). I made the decision that it would be difficult to get through a radiation treatment.
I was over at the park late this afternoon, getting some fresh air, a little exercise, and checking out some of the trees that have fall colors this time of year in Phoenix.
There's nothing like the smell of decaying leaves in the fall (in Phoenix, it's winter), right? It's such an earthy, pleasant, outdoorsy smell.
When I got home and walked through my front door it hit me. My home has lost its smell. You know how everyone's home has a certain, unique smell, right? Mine used to have a very pleasant, lived in, healthy smell. What hit me when I walked in the door was a sterile, medicinal smell that is nothing like I'm used to, and certainly not what a home should smell like.
I'm going to say that the main reason for this is that I'm no longer cooking my healthy, tasty meals. You understand that food is part of what makes a home smell the way is does, right?
Just thinking about this makes me feel sick, as does thinking too much about all of the other things I continue to go through.
Something else I've been noticing is that it's becoming harder and harder for me to read news articles about all of the sad, unfortunate, and depressing things happening around the world.
January 16, Treatment Day 19
Weight 120.1 lbs.
My white blood cell markers were down just a bit from last week (as well as platelets), so Dr. Radhi and Monica (her RN) decided to not have me do a chemo treatment today. Monica said it is totally normal for this to happen at some point during chemo treatment. If the markers are back up next Tuesday, then I will undergo a fifth chemo treatment. A sixth treatment might not be necessary or advisable.
I spoke at length today with Monica about my neuropathy, which has become noticeably worse over the past two weeks. I have no pain or tingling, just numbness, in the soles of both feet and some in the legs if I walk a short distance or stand for awhile.
I expressed my deep concern about the possibility of the neuropathy being permanent. I also expressed to her that my lifestyle, passions, and reasons for living revolve around being able to use my legs, hands, and arms (hiking, being outdoors, photography, and playing the guitar). I also told her that staying healthy and fit and eating healthy food is another passion.
Monica said that in all likelihood my neuropathy is temporary. She suggested I start using B12 drops every day, which, according to research she's done, helps with neuropathy.
January 17, Treatment Day 20
Nothing of consequence to report.
January 18, Treatment Day 21
Weight 121.6 lbs.
Speaking with my radiation doctor, Dr. Samuels, he explained that the constant phlegm production I'm experiencing is actually not mucositis, but the result of the radiation's effect on my salivary glands (it's removing the liquid component and leaving just the mucous, which, according to him, is always a part of your saliva).
In true mucositis, there is sloghing off of skin cells in the mouth, which he doesn't see.
I had two peripheral neuropathy tests done my my PCP today.
One was a "Quantaflo" test, which tests to see how blood is flowing in the arteries. I passed that test.
The second test, a "Sural Nerve Conduction Study" tests to see how siganls are flowing through nerves. That test showed that I have moderate neuropathy in my feet and/or legs.
Speaking with my PCP, Dr. Kirsten Knobbe-Lloyd, we agreed that it's most likely the cancer drug cisplatin that's responsible for this.
January 19, Treatment Day 22
Today was my 20th radiation treatment. Twenty down and fifteen to go. The next few weeks may prove to be very challenging as the continued radiation produces more side effects. Time will tell.
I noticed (and felt) several days ago that I have some minor radiation burns on the tops of my collor bones. Yesterday Dr. Samuels told me it's completely normal for the areas I'm receiving radiation. Per Dr. Samuels, I've been applying skin cream to my entire neck region to keep it moisturized.
This evening, around 6 pm, I had another bout of constipation. It seemed I had this under control, and nothing has changed regarding pain medication and my usual regimen to address it. This one was pretty bad. It took a long time to pass a huge amount of chunky, very firm stool, and once again there was some blood on it (not the first time).
So, it looks like I'll have to start taking a dose of Miralax every night rather than every other night (along with the Senna-S, which I take daily).
January 20
I decided to stop taking my once-a-day traMADol. I've been contemplating this for over a week, thinking that it really isn't necessary. The head pain I used to have for so long has been gone for quite some time, and the other discomfort I'm feeling (like soreness in the throat) is only when I put my head in certain positions.
The more significant news of the day is that today, for the first time since all of this started, I had a real, deep, heartfelt cry. It was listening to music that triggered it (music often has a way of opening me up emotionally).
The feelings were intense, and I was actually trembling slightly.
You see, I've known all along just how deeply this ordeal has been affecting me, which is why I've had to just keep my emotions at arms length, until I was ready to experience some of them.
It's hard to describe the feelings. Perhaps frightened, violated, and upset to a degree I don't think I've ever felt before are accurate.
This was a very, very healthy thing for me. I hope I'm able to experience these feelings, and all of my feelings about this as time goes on.
January 22, Treatment Day 23
Nothing of consequence to report.
January 23, Treatment Day 24
Another long chemo day today.
I had a long discussion with Amanda, Dr. Radhi's P.A., about the ongoing neuropathy in my feet and legs. I reiterated what I said to Monica last week regarding quality of life, and how much I need my body to do the things I'm passionate about and that bring me joy.
Amanda said that the cumulative dose over of cisplatin (over the entire treatment period) must be at least 250 mg. At this level or greater she said research shows the best chance of killing all the cancer and the least chance of it recurring.
At present I'm at 246 mg over four chemo days (66 mg, 66 mg 66 mg, and 48 mg).
Amanda said my white blood cell counts are the same as last week (a little lower than desirable). But, after acknowledging my concerns, she said because I did not do a treatment last week she wants me to do one today. She reiterated the fact that the chemo works in conjunction with the radiation and makes the radiation treatments more effective.
I agreed to do another chemo treatment today which will put me at 294 mg total.
January 24, Treatment Day 25
Weight 118.6 lbs. (radiation) and 122.6 (Javadi's office)
Today I had my feeding tube replaced. Some dark-colored "gunk" had collected just above the clamp.
The new tube is a bit different than the one I've been using, and not as easy to use. I'm investigating options to make it easier.
January 25, Treatment Day 26
Weight 123.4 lbs.
I asked Dr. Samuels if the CT Scans that are done at the start of each of my radiation treatments are used to monitor progress (in terms of being able to see the cancer growths shrinking). He said that those scans are used only for the purpose of alignment (aligning my body when I'm lying on the table) and nothing more.
He said when treatments are completed, three months afterwards I will have a PET Scan done to see if there is any cancer remaining.
In other words, it appears there is no ongoing visual on how effective the combined chemo/radiation treatments are in destroying the cancer. Dr. Samuels does palpate my throat and neck where I showed cancer near lymph nodes, but other than that and looking into my mouth there is no further visual inspection of the cancer at the base of my tongue (Samuels said it's just really hard to get a good look at). Yes, I find this a bit unnerving, but this seems to be the accepted protocol.
January 26, Treatment Day 27
Twenty-five radiation treatments completed, ten more to go.
The constant dry, mucous-like saliva and coughing it up all day long (followed by alkaline water rinses) is very, very tiring to say the least.
I also received a shot of filgrastim (brand name Zarxio, same drug as Neupogen). This was done in an attempt to stimulate my bone marrow to produce more white blood cells.
January 29, Treatment Day 28
Weight 118.3 lbs. (radiation)
I was feeling very "down" emotionally this past weekend. This entire ordeal has been really, really wearing on my. It's very tiring to be constantly spitting, coughing, and rinsing. At night, I have to get up every 1.5-2 hours to cough up a huge wad of phlegm.
I spoke with my Banner dietican Ann today about my feeding tube issues (I sent her a long e-mail about it on Friday).
She said she would send me a list of possible feeding tube belts I can try to keep the base of the tube tight to my abdomen (the new tube doesn't fit like the original). I've previously looked at these online, but wasn't sure which one to buy. Ann said she can't recommend anything and that I'd just have to try one.
Regarding the lack of a clamp for my new tube, Ann said sometimes tubes come with clamps and sometimes they don't. I explained to her how ridiculous it is to install a tube without a clamp. She suggested I get in touch with my contact at Aveanna (the company that provides my formula, bags, and syringes) to see if she has any ideas.
I contacted Vicky at Aveanna. She said she would send me something called a "Lopez Valve" to see if that works.
January 30, Treatment Day 29
I've noticed that my throat has become more sore over the past two days. I've been taking Acetaminophen, 500 mg, once or twice a day, which seems to keep it a level which is tolerable.
No chemo today.
January 31, Treatment Day 30
Weight 118.8 lbs. (speech)
I saw my speech pathologist Ashley today. I really like her. She's honest, down to earth, doesn't pull any punches, and is very supportive.
She said that the worst part of my radiation side effects are most likely still to come. She said that the 2-3 weeks after treatment stops is when the cumulative effect of all the treatments is usually at its worst.
Great.
I'm already at a point which is very difficult to deal with, and now it's most likely going to get worse.
Imagine having your mouth constantly producing a thick, gooey, stringy mucous. As soon as you spit it out or cough some up, it's back again. Yes, I mean immediately. It never really ever goes away.
Brushing and flossing my teeth has become something I do not look forward to. That just creates more foamy crap in my mouth.
It's impossible to get a full night's sleep because I have to get up avery 1.5-2 hours to cough up all the phlegm that's accumulated as I sleep. Oh yeah, did I mention that some of that crap just leaks out of my mouth onto the pillow or towel I have under my head when I sleep? Did I also mention that it stings on my tongue where the radiation is taking place?
I've started adding ice to my alkaline water when I rinse after spitting and coughing up phlegm. It feels good to have something really cold on the tissues in my mouth.
My throat is definitely getting more sore.
I started taking 3 Acetaminophen today, up from the 1-2 I was taking daily.
During my appointment with Ashley, at one point I just stopped, kind of looked down, and then I started to cry. I mean REALLY cry. It felt really good to let some of that emotion out.
This shit I am going through is so damn hard, and long. It feels like a marathon that never wants to end.
Ashley mentioned to my dietician, Ann, that my weight is down a bit. I spoke to Ashley about it and e-mailed Ann.
It's hard to get enough formula down to maintain weight.
If all I did was sit around all day, doing very little, going nowhere, then I could probably get the 6-7 cartons target per day (2,250-2,625 calories per day).
I agreed to try and reduce the amount of time between feedings to 3-3.5 hours rather than 4 so I can get at least 6 cartons down per day.
February 1, Treatment Day 31
Weight 119.3 lbs. (radiation)
Dr. Samuels said that healing would begin about one week after treatments end. That's one week earlier that what Ashley told me yesterday. Guess I will find out soon.
He also said it's fine to use Naproxen along with Acetaminophen (no interactions).
February 2, Treatment Day 32
Mucous and phlegm production seems to have increased. This is an issue when I receive my radiation treatments. I can only remain clamped into the mask and on the table for an even shorter period of time now before I can feel it forming in my throat. This is AFTER I've done a full throat clear and mouth rinse immediately prior to getting on the table.
February 3
I've been puzzled as to why, over the past week, my bowel movements have not returned to normal.
I stopped taking traMADol over a week ago (might be as many as two), so I stopped doing my anti-constipation protocol. Then, I had some constipation return about 8-10 days ago because I forgot that the anti-nausea meds they give you with the chemo treatments also cause constipation.
So, when the constipation started again, I went back to my usual anti-constipation protocol. Apparently, I went too far with it and I started having very loose stools. So, I stopped the protocol because I was no longer taking anything that would cause constipation (and no more chemo treatments).
Wrong!
Because my throat has been more sore this past week I've been taking one or two 500 mg Acetaminophen for pain. Little did I know, until today, that Acetaminophen can also cause constipation (showed in a simple Google search). We're talking straight up Acetaminophen (not Tylenol #3).
Now, tonight, I started taking the Senna-S again, and will take that once a day to see if it helps things normalize.
This is not fun.
February 4
I get together with my friend Cheree about once a week. We talk about what's going on with me, what's going on with her (she has some health issues she's dealing with), and whatever else comes up in our discussions.
Yesterday, we had a rather long conversation. The entire time I was spitting, and coughing, and rinsing, non-stop. Somewhere near the end of our conversation I let out a spontaneious loud yell, the likes of which I haven't done in decades. I'm sure the residents in the entire courtyard heard me. I've got to say it felt damn good to let that out.
February 5, Treatment Day 32
Because of the constant mucous, it was a challenge to get through my radiaton treatment today. Even after fully clearing my mouth and throat immediately before getting on the table, I was nearly gagging when I got off the table.
Bowel movements are still not normal, but at least things are moving.
February 6, Treatment Day 33
Still challenging to get through radiation treatment today.
February 7, Treatment Day 34
Radiation treatment not quite as bad today (a bit less mucous).
I saw my Speech Pathologist Ashley today.
I also had an appointment with a physical therapist, Colton Ruhl, for Lymphedema. He explained to me that one of the side effects of radiation is damage to the lymph nodes. To combat that, I will need to do a daily lymphatic massage protocol on my neck and upper torso, as well as come in for several therapy sessions.
He graded my Lymphedema at mild to moderate.
Did I mention that I've been sleep-deprived because of all the mucous (having to get up every 1.5-2 hours to spit and cough)?
February 8, Treatment Day 36
Weight 119.3 lbs. (radiation)
Today, Dr. Samuels said it will be two weeks before I start to see a slow improvement in my radiation side effects.
The massive amount of thick, sticky mucous in my mouth and throat is extremely unpleasant. It's nearly constant, and sometimes, when I cough up a huge thick wad from deep in my throat (which is often), it feels like I'm going to gag. And, as I've said before, it's acidic and it irritates my tongue and my throat. Sounds like fun, huh?
The mass of growth at the base of my tongue was where most of my cancer was (compared to the amount at the left and right lymph nodes). According to Dr. Samuels, with most patients it's the other way around.
I asked him specifically about my prognosis for being 100% cancer free when I have another PET Scan in three months. He said that because my p-16 markers are positive (meaning HPV-caused, as opposed to p-16 negative, tobacco-caused), my prognosis is better. When I asked him for a number (percentage) he said about 70%. I was hoping to hear something more like 90%, but he also said I have every reason to be optimistic.
February 9, Treatment Day 37
Weight 119.4 lbs. (chemo)
I had my last radiation treatment today (treatment 35). DONE!!
Below is a photograph of the mask I wore for all 35 treatments and the certificate I was given upon completion.

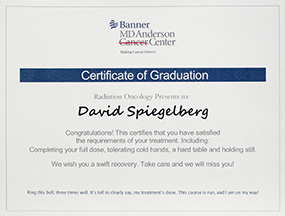
In addition I also had lab work done and had a long discussion with my chemo doctor, Dr. Radhi.
My lab work show much improved white blood cell count (2.3, up from 1.6) and normal platelet count. Dr. Radhi attributes that to the 2-week layoff from chemotherapy and the shot of filgrastim (brand name Zarxio) I received on January 26.
Dr. Radhi initially wanted me to do another chemo treatment today, but after our discussion I opted to hold off on a treatment today.
Here are the points of concern I discussed with her:
- I explained to her that according to the cisplatin numbers I discussed with her P.A. Amanda back on January 23, I have surpassed the 250 mg guideline.
- I'm done with radiation so what further incremental benefit might I get from another chemo treatment?
- I am still battling constipation, even though the only pain medication I am taking is one 500 mg Acetaminophen daily. I explained to her that it's clear that my body is hyper-sensitive to anything that might cause constipation.
- The neuropathy in my feet and legs is about the same (not worse, but no improvement).
- I am now in the most challenging part of the radiation side effects. I'm tired, weary, sleep-deprived, and the last thing I think my body needs right now is more chemicals, especially those that will increase constipation.
First, she said that the cisplatin numbers I was given are not what I actually received. Those numbers, she said, are the starting point, to which a factor is applied based on body weight and other things. In reality, she said I've received a total of 180 mg of cisplatin, not 294 mg, which I was told by Amanda (breakdown is 40 + 40 + 40 + 30 + 30 = 180 mg). According to Dr. Radhi, being at least at 200 mg total is best. When I pressed her on this, she said she couldn't give me a definitive answer because every body is different and they respond to cisplatin in different ways. In any event, she said I am just below the 200 mg threshold, which is very near the 200-250 mg level she said is minimal.
Second, she said that the radiation keeps on working in my body, even though treatments are completed. Having more chemo might help increase the effectiveness of that.
Dr Radhi was very sympathetic to my concerns and understood it was a hard decision.
We agreed to a phone conversation to revisit this next week. One thing I want to ask her in that conversation is if, supposing the PET Scan in three months shows some remaining cancer, might just a few chemo treatments at that time be sufficient to get rid of it all without further radiation?
February 10
The next two weeks or so are going to be the most challenging, in terms of symptoms, of my entire treatment.
My throat is EXTREMELY sore.
It looks like I might have a few mouth sores on my tongue, both sides.
I'm still spitting out and coughing up phlegm.
When I cough up those huge wads of phlegm from deep in my throat it irritates my throat even more, but the phlegm has to come out. At night, when I sleep, I'm still getting up about every 1.5 hours to cough up a huge wad, then I'm able to go back to bed and get some sleep after my throat irritation subsides a bit (or, maybe I've just gotten so used to mouth and throat discomfort that my mind has learned to more or less ignore it).
I know that one of the things that has helped me get to this point is distraction. Whether it's listening to music, playing my guitar (a real challenge when you're spitting and coughing all the time), working on new photo images, or watching YouTube videos, it's been an effective way to disconnect from the unpleasantness.
I also drool. It happens at night, but it also happens when I'm sitting, listening to music. If I drift off a bit, then this nasty thick, sticky mucous literally runs out of my mouth and lands on whatever top I'm wearing. Sometimes, I wrap a towel around my shoulders to catch it.
I really can't lay down on my back (that's the way I used to sleep, every night). Doing that causes the mucous and phlegm to go down my throat, and makes me gag. This affects my sleeping position as well as listening to music (which I would usually be on my back for both) - not nearly as relaxing or conducive to good sleep.
Oh yeah, have I mentioned that I am cold almost all of the time? For someone who generally runs very warm this is a bit distressing. I'm assuming it's because I've lost so much weight.
I have the thermostat set somewhere between 72 and 75, and still I'm wearing long underwear, loose cotton athletic sweat bottoms over that, and two fleece tops (and sometimes my winter weather, thick knit cap).
I relish the days when it's sunny outside and warm enough to get out for long walks in athletic shorts and a sleeveless T-shirt. We've had a lot of rain here recently, and it's been really cold (rainy and cold again today). The good news is that it will warm up for the remainder of the week with sunny skies, so I will be able to get out, get warm, and get some large doses of vitamin D.
This past week I received bills from Banner for chemotherapy and radiation treatments through December 31 of last year. I will post the amounts below over the next few days when I pay the bills.
IT FEELS LIKE I HAVE REACHED THE LIMIT OF WHAT I AM ABLE TO ENDURE.
February 14
Day 5 post-radiation and my mouth is very, very sore. I can see a sore on my tongue on the right, and yes, the constant mouthful of sticky, gooey saliva makes it sting, all the time.
I am counting the days, and somehow just trying to hang on until these unbelievably challenging symptoms begin to subside.
As I've noted, the sleep deprivation is substantial.
Beyond that, I am just plain sick of being sick and having to go through this robot-like existence day after day after day.
On the bright side, I was able to get some serious sun (vitamin D) and go for walks the past three days as the weather here in Phoenix is warming nicely.
Today, I had a phone consultation with my chemo doc, Dr. Radhi about whether I am able to do one last chemo treatment. I told her I have never been more conflicted about something my entire life.
On the one hand she says that pushing me over the 200 mg total (currently at 180 mg) might have some benefit based on statistics, but she can't say for sure because every body is different.
On the other hand I am having an extremely difficult time with the idea of allowing more chemicals in my body. And, I am VERY concerned about the neuropathy in my feet and lower legs.
During our discussion I said that the neuropathy hasn't gotten worse, but during my walk today (after our discussion) it felt like it is getting worse. And, my ankles and lower legs have become noticeably swollen.
I messaged my PCP about this. She said I should try some compression socks and try to keep my feet elevated as much as possible.
Of course, the big question is whether this is just a temporary side effect, or whether it is not. Doing another chemo treatment might make it worse, but again, no one can say for sure.
What I do know for sure is that losing the use of my legs, as I've known it, would be a HUGE blow to my quality of life. How would I put a camera pack on my back and go out and take photographs?
At the end of our discussion I reluctantly agreed to do one more chemo treatment. But, it depends if they can get the treatment scheduled (since this is last minute), and as I mentioned, the neuropathy in my legs is a HUGE concern which might be the deciding factor.
I was able to bring most of my houseplants back into my living space today. They have been out on my patio for quite a while now. So, yes, at least that is some step in the direction of a return to normalcy.
February 15
Up early this morning, around 7:00 am. I was up twice during the night. The second time, around 4:00 am, I did a long steam treatment to help loosen up phlegm in my throat and congestion in my sinuses. I coughed up 3-4 large wads of phlegm (which really irritates my throat) and I was able to forcefully blow my nose a bunch of times and get some clearing in my sinuses. When I blow, I see very small bits of blood and varying amounts of red liquid, but I haven't had an actual nosebleed in over a week.
I think I might have a case of sinusitis or an actual sinus infection (although I don't have a fever). It's possible it's allergies, but what I'm experiencing now is way more different than the typical allergy symptoms I've had over the past several years.
Despite all this, it feels like I was able to at least get some halfway decent sleep.
February 16
Weight 120.1 lbs. (chemo)
Dr Radhi's staff was unable to schedule me for another chemo treatment, but I did have an in-office appointment with Dr. Radhi today.
She asked me again if I still wanted to schedule one last chemo treatment for next week. She confirmed that at this point the effectiveness of it would be less because it would be over one week out from my last radiation treatment. I explained to her my concerns and current symptoms and decided to not do another treatment. My feeling is that one more treatment at this point is most likely not going to make a difference in my outcome. If it turns out I still have some remaining cancer in three months (after the Pet Scan), then I will just have to accept that and do whatever additional treatments are necessary.
As on outsider you might think this was a bad decision. Keep in mind that you haven't lived through my cancer ordeal. Even if you've been reading this post on a regular basis, you still don't really know or understand just how difficult what I am going through has been. Reading about it and experiencing it are two entirely different things. Yes, I am a very strong and tenacious person, but I'm still human. As I said recently, I have reached what feels like the limit of what I can endure.
In my meeting with Dr. Radhi today I expressed my concerns about my continuing symptoms: 1) extremely sore throat, 2) constant thick, sticky saliva/mucous in my mouth, 3) huge, thick wads of phelgm which I cough up constantly, 4) sinus issues, and 5) the possibility that I have been aspirating a small amount of phlegm, which could result in pnuemonia.
Regarding the first three, she said these are all normal post-radiation side-effects.
Regarding the sinus issues, I explained to her that I get intermittent dripping of clear liquid from my nose, and that this is not a typical symptom of my allergies. I also said I was concerned that maybe I have sinusitis, or possibly a low-grade sinus infection, and that maybe this was contributing to the huge wads of phlegm I've been coughing up.
I had no fever and she didn't think I had a sinus infection, but she suggested I go on a 5-day regimen of antibiotics just to be sure.
Regarding the aspiration, she checked my lungs with a stethescope. She said my breathing was normal and she couldn't hear any sounds coming from my lungs. She had me do a chest x-ray (before I left her office) which showed nothing of concern.
I also told Dr. Radhi that it feels like my neuropathy has gotten somewhat worse. This, and the fact that I still think I might have a low-grade sinus infection were two fadctors in my decision to not do another chemo treatment.
Later in the day, I took a long walk. Yes, the neuropathy is definitely somewhat worse, and my legs felt noticeably tired, which is not normal at all for me when taking a one-mile walk.
February 17
I was up three times during the night coughing up massive amounts of phlegm. Again, I did a long steam treatment which helps loosen things up.
When the radiation techs said my side effects were going to get worse before they get better, they weren't kidding. This is absolutely insane.
February 22
It seems that I'm coughing up phlegm somewhat more frequently. I still wonder if this isn't at least partially related to what's going on in my sinuses.
Yesterday and earlier today I was able to really clear my sinsuses with some very deep, forecful nose blowing several times with no nose bleeding whatsoever. It feels like maybe whatever is going on there (deep in my sinsues) might be started to clear.
Two days ago I tried doing some pushups as part of my at-home exercise routine. I struggled to get three! At the gym, when I'm fully warmed up I usually do two sets of 15 without a problem. This shows just how much strength (and muscle mass) I've lost.
I've been doing my at-home exercise routine only sporadically. Why? Because it takes physical and mental/emotional energy to do it. My entire cancer ordeal has done a "number" on not only my body but my mental/emotional state as well. Now that I am through treatments and in the recovery phase, it's time to get back to a regular at-home routine until I'm able to actually get back to the gym (which won't happen until all of this spitting and coughing subsides).
February 26
I was able to get out and ride my bicycle yesterday (Sunday) and Friday for the first time in many months. Friday was just a "test drive" so to speak, maybe a mile and a half or so. Yesterday was more vigorous, I would say 4-5 miles with some up and down terrain. For sure I have lost strength and stamina, but it sure felt good to get out on my bike again. I'm going to make this a regular part of my fitness routine going forward until I can get back to the gym.
I'm continuing with my "mini" workouts at home.
I've been out doing photography twice over the past 3-4 days. The way I do photography is pretty labor-intensive, but it felt REALLY good!
In short, I'm feeling strong enough to do some of the things I used to do to help get my life back to normalcy.
The jury is still out on the neuropathy, but the good news is that so far it hasn't kept me from doing the things I love to do.
I decided to take the antibiotic I requested from my chemo doctor because my sinuses are still a bit of a problem. Today is day 4 of the 5-day regimen. If this doesn't help relieve symptoms, then I will start taking Cetirizine again thinking perhaps it's allergies.
The spitting and coughing might be relenting just a tiny bit (keyword "tiny"), but it's still very annoying and just a nuisance.
All in all, lots of good news!
February 27
Weight 122.1 lbs. (speech)
I had three appointments at Banner today.
First, to see my Lymphedema PT Colton, who did a fair amount of lymphatic drainage massage on my neck and upper body. He took measurements again and said that they show some improvement since my last visit 2-3 weeks ago (less swelling).
Second, to see my Speech Pathologist Ashley. We talked at length about my mucous/saliva spitting and coughing. The spitting of thick, somewhat dry foamy mucous/saliva continued throughout our conversation (talking seems to make my mouth create more mucous/saliva).
Ashley said I should start drinking small amounts of water again (4-8 ounces per day) and to gargle with baking soda and salt to see if that helps with the mucous/saliva, and to just get me swallowing again. I was able to drink about 4 ounces of water while in her office. I was able to swallow it okay, but every swallow caused the same pooling that I've experienced for at least a year now (which causes me to clear my throat multiple times after each swallow).
She cautioned me regarding possible aspiration, saying if I start to feel anything going on in my chest (possible lung infection), to immediately stop my water intake by mouth.
She scheduled another Swallow Test for March 11, which she will perform. The results of this Test will tell us if I'm still aspirating, and if so how much.
The big, $64,000 question, of course, is how much overall relief I am going to get from my dysphagia from the cancer treatments. It's still possible (and likely in my view) that there are other things causing it. Most likely, once my throat has full healed from the radiation treatments, I will undergo an upper esophagus dilation to see if that helps with the pooling.
Third, I saw Dr. Samuels for a post-radiation treatment checkup. Overall he thinks I'm doing really well with healing. I still have a sore area on the left underside of my tongue, and my tongue still deviates a bit to the left when I attempt to stick it straight out. Samuels said that could be from scar tissue, but it's impossible to know for sure. He confirmed that we will do another Pet Scan on or around May 7 (three months after my final radiation treatment).
March 1
Second session with my Lymphedema PT Colton.
March 3
I finished my 5-day antibiotic regimen of Azithromycin back on February 27 (for a possible sinus infection). I can't say I've felt any significant difference, although my sinuses seem to have cleared somewhat over the past week.
This past Thursday, February 29, for the first time in several months I joined our Thursday chess group at the Granite Reef Senior Center in person. It felt really good to be back with my "chess buddies" even though I was spitting up mucous/saliva pretty much non-stop and had to get up and go outside several times each hour to cough up phlegm.
When you have this mouth and throat mucous/saliva condition you must take something to spit in everywhere you go, otherwise you can't even have a conversation with a store clerk, or whatever because your mouth is full of crap. And, of course, you have to explain to some of them why so you don't appear as some kind of mentally-deficient idiot!
Did I mention how much I dislike brushing my teeth since all of this nasty mouth and throat stuff has gotten into "full gear?" I brush my teeth in two steps - first the lower, then the upper because I end up with such a nasty mouthful of foamy mucous that it makes me gag.
Regarding the mucous/saliva, over the past week to 10 days it has gotten more dry, sticky, and gooey, which is even more disgusting and unpleasant.
I would say however, that over the past two days it does seem like the amount and frequency of my spitting has been a little less.
I have been really focusing on my swallowing exercises and being very diligent about forcing myself to drink small amounts of water with each feeding the past few days. I'm also back to lots of mouth rinsing with alkaline water and gargling several times a day with baking soda and salt (suggested by my speech pathologist).
I had gone several weeks without drinking even one drop of water by mouth because the mucous/saliva and phlegm was so bad, and trying to swallow anything meant swallowing some of that crap as well. Now, with another Swallow Test coming up a week from Monday, it's time to really work hard on doing everything I can to see how much of my swallowing ability I am able to regain.
March 7
I've been getting out on my bicycle and getting regular small doses of sun (vitamin D). I am able to do 5-6 miles with significant up and down terrain which makes me really work my legs. I'm also continuing with my at-home workout routine. My plan is to go back to the gym one day this weekend with a spit cup in hand.
I've been diligently doing my swallowing exercises three times each day, and that, along with all of the other good things I'm doing, has already made a noticeable difference. I am now able to swallow fairly large amounts of water with no apparent aspiration (that I can feel). Yes, I'm still getting some pooling, but it seems like it might be a bit less than before. This comes at a time when I really need to be hydrating my throat throughout they day because of how dry and sticky the mucous/saliva situation is.
I'm still spitting and coughing (really dry, really thick and sticky), but the volume of phlegm seems to be somewhat less, and I've been able to get somewhat better sleep at night.
March 8
I had my third Lymphedema session with PT Colton today. He noticed, before taking measurements, that my neck looked a little swollen. Measurements confirmed that I was more swollen than my last session. It might be because I have not been doing my at-home drainage protocol this past week (because I've been working really hard on swallowing exercises).
After Colton worked on me (spent most of his time on my neck) the swelling was less.
March 10
Today I went back to the gym (first time there since mid-November of last year). I took my "spit cup" with me, of course (because I must have a "spit cup" wherever I go).
Yes, it felt good to be in familiar surroundings and back doing what I love. Yes, it was obvious that I have lost quite a bit of strength, muscle mass, and flexibility. This is the start of a long road back to where I was before all of this dyshphagia and cancer started.
March 11
I had another Swallow Study done at Banner hospital.
The technician doing the test, Katherine, had me swallow three different things: 1), just water, 2) thickened water, and 3) firm pudding (no dry food).
After the test we discussed the results. As far as aspiration, there has been a big improvement since my last Swallow Study last fall! There was the tiniest bit of liquid that you could see trying to "backwash" its way into my windpipe on one or two of the images, but it was unclear if it even entered my windpipe. Katherine noted that this appears to be happening only when I cough to clear the pooling in my throat, not on my initial swallow attempt.
Of the two times she had me swallow pudding, the first time it went down quite well. The second time, not so much.
One thing to factor into this Test is that my mouth and throat are still coated with thick mucous/saliva. I suspect that when that fully clears up, it will help my swallowing to some degree.
Katherine said that I could benefit from a dilation of my esophagus.
Now I wait to hear from my Speech Pathologist Ashley to see if I am clear to start swallowing any soft foods.
My water intake via mouth is now around 12-16 ounces per day, and I am able to swallow fairly large amounts in one gulp. Just 10 days ago it felt uncomfortable to swallow even small sips.
The neuropathy in my feet and lower legs is about the same - no change.
The thick, dry, sticky mucous/saliva continues, although it seems like the amount continues to slowly decrease. For some reason, when I talk and have a conversation with someone, it gets really bad and it's non-stop (it's been that way for quite some time).
I've been doing baking soda/saline mouth rinses and gargling at least once a day, and I'm still doing steam treatments to sooth my sinuses (still seeing small amounts of blood when I blow my nose) and to help loosen mucous/saliva in my throat.
March 13
I had my fourth Lymphedema session at Banner today. This time I worked with a different therapist named Suzanne.
She said that overall my swelling wasn't all that bad, but she did note that the back of my neck on the left and the front of my neck on the right did have some swelling. She spent a lot of time doing lymphatic massage on my entire neck.
She said that it's possible I will have to continue doing at-home lymphatic massage for a long time, possibly for life, because of the damage done to the lymph system by radiation treatments.
She also said that if possible, I should try and wear the compression "sleeve" I was given at night to help keep swelling down. She also said that in the morning is when the swelling is usually worse (because you've been lying down without the help of gravity all night while asleep), so doing at-home massage is best done early in the day.
The big news of today is that I received the "green light" from my Speech Pathologist Ashley to go ahead and start snacking on foods like yogurt, applesauce, pudding, and even blender-ized soups. She said that after reviewing the results of my test on Monday, she sees no aspiration. This is really good news!
She also gave me the "green light" to drink as much water as I can, saying that the more I drink (and swallow) the sooner things will get back to normal.
Time to go shopping at Fry's!
March 20
I had my fifth Lymphedema session at Banner today. At the start of each session Colton, my therapist, takes a set of measurements of my face, jaw, neck, and head. He then adds these up, the sum of which is used to compare week-to-week to see how I'm progressing with reducing the swelling in my neck. Today, I had just a little bit less swelling than last session.
I've been wearing a neck compression sleeve every morning for about 45 minutes over the past week (and not doing the at-home lymph drainage protocol because I'm still focused on swallowing). This may be why I've been able to keep the swelling down over the past week.
Colton confirmed that managing Lymphedema for radiation patients is usually a lifelong endeavor and not something that will just go away with time.
Regarding swallowing, I'm still doing a full set of swallowing exercises three times per day (while I'm feeding) and it's made a big difference.
Since last Friday (March 15) I've been eating small amounts of soft foods like yogurt, applesauce, and blender-ized soup. The food is going down reasonably well, but I do need to wash it down with water. I'm able to taste everything, so that's good news. I must say that blender-ized Progresso vegetable soup at room temperature never tasted so good! I'm scheduled to see my Speech Pathologist Ashley on April 2 where we will discuss my swallowing progress. I hoping she might say I'm ready to try eating a greater variety of foods.
I've been to the gym twice the past week (third time there), accompanied by a "spit cup" of course, and was able to get out on my bicycle for a 5-6 mile ride yesterday, in addition to getting out for walks in the sun.
I'm also still getting out and doing quite a bit doing photography. This time of year there's a lot to photograph!
The neuropathy in my legs and feet is about the same.
The coughing and spitting of thick, sticky saliva/mucous continues, although it is ever so slowly improving.
I've been able to sleep better at night because of less saliva/mucous.
March 23
I've had a couple of new developments over the past week.
First, I've developed a low, noticeably guttural sound in my voice. My concern is that maybe this is the start of some sort of bacterial infection. The stuff I've been coughing up from deep in my throat is still clear (no coloration), I don't have a fever, my breathing and wind is normal, and I feel just fine.
Second, just yesterday, I started to feel some pain and discomfort in my upper chest, about 2-3 inches above my right nipple. This came on suddenly. Today, it hurts in that area when I cough or blow my nose. I doubt this is lung-related because it came on so suddenly.
It's possible I somehow tweaked a pectoral muscle putting on or taking off my photography pack, but since I've been using that pack over the past 3-4 weeks, it would seem odd that all of a sudden that would cause a problem.
Yesterday I started working with a physical therapist for pain and discomfort in my left upper arm (which has been going on for the past 4-6 months). I suppose it's possible that the initial exercises I did while at PT yesterday might have caused what I'm feeling in my chest, but the amount of weight I used was very low so that's doubtful.
My plan is to stop the intake of soft food (on the outside chance I'm aspirating just a little) and take Naproxen twice a day for a few days and see what develops. I think it's possible that what I'm feeling is the result of leakage of a small amount of saliva/mucous down my windpipe at night when I sleep.
Looking ahead, although my overall cancer recovery is going really well, I"m certainly not "out of the woods" just yet.
First, assuming the PET Scan I have done in early May is clear and shows no signs of cancer, then I will have to schedule a time to have my chemo port and feeding tube removed. There will be some recovery time from the removal of the feeding tube because that tube inserts directly into my stomach through my abdomen.
Second, I have what appears to be an inguinal hernia on the left side. Most likely I will have to have this fixed, soon, and that will involve recovery time.
Third, most likely I will need to have a dilation performed on my esophagus to help with my dysphagia. When cancer was discovered, it "muddied the water" about what was actually causing my dysphagia, but I think it's clear at this point of recovery that the cancer alone was not responsible for all of my swallowing issues.
Factoring all of that into the equation of my upcoming life, and assuming I have a clear PET Scan, I would say it's going to be sometime in mid-summer before I am back and "fully functioning" as far as my body is concerned.
I was told by someone during my treatments that being treated for cancer is a marathon. That person wasn't kidding.
March 24
As if I don't have enough on my plate already, today I am reporting another new development.
About six weks ago I noticed a very small lump on my left jawbone (beneath my ear). I meant to mention it to Dr. Samuels but somehow it didn't get added to the written list I made for my subsequent appointment with him (I had a bunch of other things on that list). For some reason, at the time I wasn't overly concerned about it and thought it might just go away on its own.
Today, palpating the lump, I would say it has grown a bit in size and it feels like it extends forward a bit.
I did some research and found an article on the Mayo Clinic website that discusses jaw tumors and cysts. After reading through the article, it's clear that I need to report this to my oncology team tomorrow, right away.
March 25
I sent a message to Dr. Samuels describing my concern about the small lump on my left jaw. I received a call back and scheduled an appointment with Dr. Samuels for tomorrow morning.
Whatever pain I was feeling in my upper chest is gone, so today I resumed supplementing my tube feedings with soft food.
March 26
Weight 123.7 lbs. (radiation)
My weight is up a bit - that's good news!
In my appointment with Samuels we discussed the following topics:
- Lump on my jaw: Samuels isn't concerned and thinks it might just be part of my normal body structure. Although he didn't mention this, I'm thinking it might be that he's correct, and that my weight loss is now making the lump noticeable. He said I can have a CT Scan done if I'm at all concerned. I said yes, I was given an order for a CT Scan, and I will call to schedule it. I will send a message to Samuels via the Banner portal with the results.
- Upcoming PET Scan: 12 weeks from the date of my last radiation treatment is May 3. I was given an order for a PET Scan, and I will call to schedule it for May 3 or shortly thereafter. I will also call Samuel's office to schedule a follow-up appointment with him several days after the PET Scan.
- Deep, guttural sound in my voice: Samuels said he thinks it might be caused by residual swelling (from the radiation) in my larynx. I'm not sure if I agree with that assessment, but time will tell. Samuels checked my lungs and heart with a stethecsope and everything was normal. My temperature today was normal (no fever).
- Flouride trays: I asked Samuels if I can start daily flouride treatments, he said yes. He said to brush and floss first, then do the flouride treatments (only need to keep trays on for three minutes, and don't eat or drink anything for 30 minutes afterwards).
- Today's appointment means my appointment with him for April 18 is not necessary.
The constant saliva/mucous has subsided quite a bit recently. I was able to see Dr. Samuels today, and have a PT session for my arm/shoulder without a "spit cup." I still have accumulations deep in my throat, but they are definitely less frequent. I think that because my saliva is getting closer to normal, I am able to swallow it (without even thinking about it) most of the time.
March 28
I had my sixth Lymphedema session at Banner yesterday. My overall measurments increased one cm over the past week, but Colton doesn't feel it's enough to warrant any change in protocol right now.
After meeting with my PCP yesterday, I decided to restart my allergy protocol. The hope is that not only will it alleviate the small amount of blood I sometimes see when I blow my nose, but also to see if it decreases or eliminates the wads of phlegm that I still sometimes cough up from deep in my throat. I started last night withe Cetirizine and continued today with a sinus flush and Flonase.
The consistency of my saliva has been changing rather quickly over the past several days, for the better! Tonight, especially, it feels like it's getting clsoe to normal. I've been making an effort to "wean" myself off of the "spit cup" over the past several days and I'm making great progress!
March 29
Weight 121.4 lbs. (chemo)
I had blood work done and had an appointment with my chemo doctor, Dr. Radhi today.
Dr. Radhi said all of my blood work looks good and is normal.
I had asked Dr. Radi to include thyroid markers in my blood draw yesterday. I viewed the results on the Sonora Quest labs website and sent the information to my PCP to see if my thryoid medication needs adjusting.
March 31
Over the past two days I've been trying a few different foods to see how well I'm able to swallow them. I've tried soup (paritally blender-ized) from Saigon Bowl, sliced deli turkey, vegetarian California rolls, and soft, chewy granola bars. I was able to swallow all of those foods with minimal effort!
One thing I noticed is that when I chew, the food in my mouth is fairly dry because (I assume) my salivary glands are still not producing enough of the viscous fluid they normally do. However, I was able to swallow those foods, even without drinking water to help flush them down. I'm thinking that when my saliva gets back to fully normal, it will make all types of food even easier to swallow.
As of this weekend, I have "officially" retired my "spit cups." What a relief, and what an accomplishment! I thought this day might never come!
April 2
Early this morning I had a CT Scan done on my neck to see if the small lump on my left jawbone is a concern.
A couple of days ago I was able to eat a 6-inch tuna sub sandwhich (with all the veggies) with no difficulty.
I met with my Speech Pathologist Ashley today. She was surprised at how much progress I've made with swallowing "normal" food!
We discussed the criteria for ending the use of my feeding tube. According to her, if I can maintain my current weight for two weeks without the tube (or with minimal tube use), then I'm ready to have the tube removed.
We also discussed my long-term weight goals. I told her I was about 132-135 lbs. before the dysphagia and cancer happened. I said I would like to get back to that level, and that getting back to the gym on a regular basis will be necessary for that to happen. She suggested that 130 lbs. might be a good shorter-term goal.
Ashley lifted all restrictions on my diet and said to keep using the tube feedings (at lesser frequency) for at least a while to ensure I'm getting proper nutrition.
When I eat, because my saliva is still not fully normal, I have to sip a very small amount of water with most foods as the food is still in my mouth. I also have to use a water "flush" to get every last bit of food down my throat after I swallow.
April 4
In a phone call, I reviewed the results of the CT Scan with Dr. Samuels. He said that all looks good. The CT Scan found nothing abnormal with the lump on my jawbone. I told Samuels that I would keep a close eye on the lump and let him know if it gets larger over time.
The other good news from the CT Scan is that regarding the base of my tongue and the lymph nodes in my neck (where my cancer was), there is no "residual measurable mass." In other words it appears at the moment that all of the cancer is gone.
For the first time in many months, I made my first home-cooked meal! I made one of my signature breakfast dishes: two scrambled eggs mixed with lightly sauteed veggies, a side of cottage cheese, and one half of a bagel with a small amount of peanut butter. Yes, it took my a while to eat all of that, but everything went down just fine!
Regarding taste, I would say that my taste buds are "firing" at about 70%. I can taste everything I'm eating, and it tastes really good, but it's still not 100%.
April 5
Weight 122.2 lbs. (Banner PT)
April 7
Weight 122.4 lbs. (L.A. Fitness)
April 12
Weight 124.5 lbs. (rehabilitation)
I had my seventh Lymphedema session at Banner today. My overall measurments increased five cm since my last session. Colton thinks it might be related to my weight gain or possibly an increase in my sodium intake. He wants to see me once a week over the next month to monitor my progress.
Over the past week I've been eating lots of food! About 90% of my intake is now real food, supplemented by occasional tube feedings. I'm eating all of the things I used to eat prior to my cancer diagnosis, and in sizable quantities.
It takes me a fairly long time to eat a meal because I have to sip small amounts of water with anything dry or sticky (because my saliva is still "dry"). I also have to concentrate on chewing and swallowing, much like I was doing pre-cancer with dysphagia. And, I need to wash each mouthful down with a small amount of water to help the bolus move down my esophagus. This may improve over time, but I think most likely it means I will need to have a dilation performed on my esophagus.
I've noticed that early in the day I still feel tightness in my jaw and chewing muscles. Because I'm now doing much less tube feeding, I'm been doing less swallowing exercises. Before, when all my nutrtion intake was via tube, I was able to do my swallowing exercises during my feedings. Now, because I'm eating like a normal human being, doing the swallowing exercises is not as "convenient" (for lack of a better word). But, it's important that I keep doing them because soft-tissue and radiation fibrosis is very common with tissue that has been radiated.
I did some online research regarding radiation fibrosis and found two very informative articles, both from the National Library of Medicine/National Center for Biotechnology.
Here are some key quotes from the first article entitled "Radiation-Induced Fibrosis in Patients with Head and Neck Cancer: A Review of Pathogenesis and Clinical Outcomes":
RT [radiation therapy] presents with many acute and long-term complications, several manifesting months to years following treatment. Specifically, fibrosis and scarring of the surrounding skin and musculature is a common adverse effect occurring up to 1 year after completing treatment, and worsening over time. 2 This can be the attributed to a chronic inflammatory process due to repetitive injury induced by RT.
This process can manifest as neck stiffness, trismus, and pain and may be associated with lymphedema often leading to decreased quality of life for long-term cancer survivors of head and neck cancer.5
The severity of radiation fibrosis in the head and neck area is affected by several factors and tends to be worse in older patients, larger tumors, higher radiation doses, treatment volume, and in patients who have undergone other treatment modalities such as surgery and chemotherapy.
Even in patients treated with modern techniques, such as intensity-modulated radiation therapy (IMRT), the occurrence [of grade-2-or-higher neck fibrosis] still remains as high as 30%.
One common side effect of fibrosis in the head and neck area is shoulder dysfunction. This can be attributed to capsulitis as well as tendinitis and hardened tissues limiting the range of motion of the shoulder joint. This is usually managed with physical therapy and steroid injections into the joint to relieve pain and improve range of motion. 30 Radiation may also cause dystonia and spasms of the neck musculature. This can lead to contracture and fixed neck positions, or weakness and difficulty supporting head posture. Furthermore, fibrosis in lingual muscles and constrictor muscles may limit tongue mobility and swallowing. Trismus, which is a dysfunction in motion of the tempo-mandibular joint (lock jaw) is also a side effect attributed to the assimilation of fibrotic tissue in the joint and surrounding musculature, particularly the lateral pterygoids, often causing poor oral hygiene and nutrition as well as decreased quality of life. A suggested parameter to define trismus is a mouth opening of less than 35 mm.
Early physical therapy focusing on range of motion has been shown to decrease the incidence of trismus.
Lymphedema is also a common side effect due to radiation fibrosis and may be subdivided into internal and external components. It has been associated with worse quality of life and is more frequent in patients receiving multiple treatment modalities including surgical dissection and re-exploration surgical interventions.
Here are some key quotes from the second article entitled "Radiation Fibrosis Syndrome: the Evergreen Menace of Radiation Therapy":
Radiation fibrosis syndrome (RFS) is a progressive fibrotic tissue sclerosis with various clinical symptoms in the irradiation field. It is usually a late complication of radiation therapy and may occur weeks or even years after treatment. It may affect the musculoskeletal, soft tissue, neural tissue, and cardiopulmonary systems. RFS is a serious and lifelong disorder that, nevertheless, may often be prevented when identified and rehabilitated early...Management of this syndrome is a complex process comprising medication, education, rehabilitation, and physical and occupational therapy.
Highly conformal RT techniques such as IMRT [the type of radiation therapy that I had] and IGRT have resulted in minimal acute and chronic side effects compared to 2D and 3D techniques.
One of the most important late effects of RT affecting a patient's quality of life (QOL) and causing significant morbidity is radiation fibrosis syndrome (RFS), which may occur in the skin, subcutaneous tissue, pulmonary system, gastrointestinal and genitourinary tracts, and in any other organ within the radiation field. Radiation injury triggers inflammation and ultimately stimulation of the production of myofibroblasts from differentiated fibroblasts that in turn produce excess collagen and different constituents of extracellular matrix, aided by the reduced secretion of remodeling enzymes. Subsequent fibrosis reduces tissue compliance and causes cosmetic and functional impairment that significantly impacts the QOL in the majority of cancer patients, and particularly those with head-and-neck (H and N) cancer.
The advent of IMRT and IGRT has allowed maximum tumor dose and minimal exposure to normal tissues based on the process of dose painting, thereby reducing radiation-induced fibrosis (RIF).
RFS is generally a late complication of radiation that may either not manifest clinically for years after treatment known as delayed RFS, within a year as chronic RFS, or even during treatment in few cases as acute RFS.
RFS causes shortening and contracture with loss of elasticity of the tendons and ligaments, thus resulting in restricted joint mobility, joint swelling, and loss of functionality.
April 14
Weight 125.4 lbs. (L.A. Fitness)
April 15
I received a response from my Speech Pahologist Ashley regarding a few questions I asked her via e-mail. Here's the text of Asley's response:
Hello!
Thank you so much for the update! I will let Gwin know you do not need to renew your order [for formula and feeding tube supplies].To answer your other questions:
In terms of taste, most say it continues to improve with time. Very few say it gets back to 100%. Improvement over 12-18 months following treatment are reported.
Yes, fibrotic changes are a lifelong reality. We can't undo the changes that radiation inflicts on tissues, however, the stretches, exercises and swallowing food itself do help to preserve your flexibility. This is why we start you on the exercises so early and encourage you to continue them as able. Fibrotic changes typically begin to develop roughly 3 months after treatment is completed, although some folks do feel things changing earlier and others feel very few changes. I very much appreciate how in-tune you are with your body and I know if you feel changes you will bring them forward to address them rather than waiting for bigger issues to develop. I would be mindful of your jaw, as we talked about before I recommend you open, stretch and hold a few times every morning and evening. I will re-measure you when you return to clinic.
Your tongue and lip range of motion are intact (two major players in speech articulation), so I suspect your speech changes are related to dry mouth if experiencing that, or possibly even due to changes in motor behaviors that developed over months of having to spit out copious amounts of mucous. Now if what you're noticing is more of a change of resonance or the way your voice sounds, that may be related to tissue changes following radiation. I can take a look at that when you come back as well.
Again, I can't believe how well you are doing, keep up the excellent work!!
April 16
Weight 126 lbs. (Banner PT)
April 17
Weight 125.5 lbs. (rehabilitation)
I had my eighth Lymphedema session at Banner today. My overall measurments increased three cm since my last session. Colton still thinks my recent increases might be related to my weight gain. The plan is for me to try to wear the compression neck sleeve for a longer period of time each day (I've been doing about 45 minutes each day) and to try and do the at-home lymph drainage protocol more often (I explained to Colton how difficult it is, time-wise, for me to do the at-home protocal now that I'm making my own meals and eating real food again).
Out-of-pocket Medical Expenses
| DATE | SERVICE | OUT-OF-POCKET |
| 03/21/24 | HonorHealth swallowing therapy (May 2, 2023 through May 31, 2023) | $20.00 |
| 03/12/24 | Banner (Radiation treatments 01/02/24 through 02/01/24, date of service on bill 01/02/24, total of $55,094.00 billed to insurance) | $1,802.20 |
| 03/12/24 | Banner (Radiation management/Dr. Samuels, service date 01/26/24, total of $491.00 billed to insurance) | $60.00 |
| 03/12/24 | Banner (Radiation management/Dr. Samuels, service date 02/02/24, total of $491.00 billed to insurance) | $60.00 |
| 03/11/24 | Swallow Study co-pay | $15.00 |
| 02/22/24 | Banner (Chemotherapy treatments through 12/31/23, date of service on bill 12/25/23, total of $3,805.80 billed to insurance) | $81.93 |
| 02/22/24 | Banner (Radiation treatments through 12/31/23, date of service on bill 12/17/23, total of $17,324.00 billed to insurance) | $330.00 |
| 01/26/24 | Fry's (Distilled Water) | $2.58 |
| 01/26/24 | Dollar Tree(chip clips) | $1.35 |
| 01/20/24 | Fry's (Liquid Guaifenesin) | $11.20 |
| 01/20/24 | Fry's (Distilled water) | $9.09 |
| 01/16/24 | Sprouts (Vitamin B12) | $6.56 |
| 12/28/23 | Kroger brand Depends | $10.79 |
| 12/26/23 | Senna-S tablets (constipation) | $3.99 |
| 12/26/23 | Liquid Mucinex | $7.94 |
| 12/25/23 | Liquid Mucinex | $7.94 |
| 12/18/23 | Milk of Magnesia | $5.71 |
| 12/17/23 | Miralax | $14.99 |
| 12/16/23-12/17/23 | HonorHealth ER (severe constipation, 11/25/23) | $90.00 |
| 12/15/23 | Aquafor (healing ointment) | $6.99 |
| 12/13/23 | Allergen Air Filter, anti-bacterial cleaning supplies | $23.20 |
| 12/11/23 | Liquid Guaifenesin | $8.78 |
| 12/06/23 | Radiation Simulation at Banner | ??? |
| 12/05/23 | Appointment with Speech Pathologist at Banner | ??? |
| 12/05/23 | Mucinex DM, Ginger Ale | $15.21 |
| 12/06/23 | Box of 25 masks | $10.36 |
| 12/03/23 | Dulcolax | $8.36 |
| 12/02/23 | Prune Juice, Apple Sauce | $9.14 |
| 11/28/23 | Lab Work and appt with Dr. Radhi at Banner | ??? |
| 11/27/23 | Appointment with Dietician at Banner | ??? |
| 11/25/23 | HonorHealth ER (severe constipation) | $70.00 |
| 11/24/23 | HonorHealth Urgent Care | $40.00 |
| 11/22/23 | Delivery of food and supplies by Aveanna HealthCare | ??? |
| 11/22/23 | Dental Fluoride Trays | $400.00 |
| 11/22/23 | Gel Kam Flouride | $20.00 |
| 11/21/23 | Fry's (Ondansetron 4 mg) | $4.15 |
| 11/21/23 | Surgery at Banner (port and feeding tube) | $175.00 |
| 11/17/23 | Modified Barium Swallow X-ray test at Banner | $25.00 |
| 11/16/23 | MDC at Banner (Dr. Samuels) | $10.00 |
| 11/16/23 | MDC at Banner (Dr. Radhi) | $10.00 |
| 11/15/23 | Pet Scan at SimonMed | $225.00 |
| 11/09/23 | Phone appointment/follow-up with Dr. Javadi | ??? |
| 11/02/23 | Biopsy at Banner ($150.00 paid on 12/10/23) | $165.00 |
| 10/26/23 | Appointment with Head and Neck Surgeon Dr. Javadi | $10.00 |
| 10/24/23 | Speech pathology at Banner | $40.00 |
| 10/24/23 | First appointment at Banner with NP | $10.00 |
| 10/19/23 | Appointment with ENT at Enticare | $10.00 |
| 10/13/23 | Cervical CT Scan at SMIL | $50.00 |
| 10/03/23 | Appointment with Kelli Patterson at Sonoran Spine | ?? |
| 09/25/23 | Banner Physical Therapy (6/20, 6/26, 7/05) | $60.00 |
| 09/25/23 | MRI of cervical spine at SimonMed | $50.00 |
| 09/15/23 | Appointment with PA at Scottsdale Sinus and Allergy | ??? |
| 08/29/23 | Appointment with Kelli Patterson at Sonoran Spine | ??? |
| 08/11/23 | Appointment/eval with Dr. Secrest (chiropractor) | $159.36 |
| 06/07/23 | Follow-up appt with Dr. Gary Reese at HonorHealth | $20.00 |
| 06/05/23 | Brain MRI at SMIL | $50.00 |
| 05/04/23 | Appt with Dr. Gary Reese at HonorHealth | $20.00 |
| 05/03/23 | HonorHealth swallowing therapy | $20.00 |
| 04/27/23 | HonorHealth swallowing therapy | $20.00 |
| 04/18/23 | HonorHealth swallowing therapy | $20.00 |
| 04/15/23 | HonorHealth swallowing therapy | $20.00 |
| 04/02/23 | Valley ENT | $20.00 |
| 02/16/23 | Brain CT Scan at SMIL | $70.53 |
| 02/12/23 | HH MBS (swallow) Test | $20.00 |
| 02/08/23 | Valley ENT | $70.00 |
| 01/26/23 | Sinus CT Scan at SMIL | $50.00 |
| 11/15/22 | EGD at Scottsdale Gastroenerology Specialists | $125.00 |
| 11/15/22 | Scottsdale Gastroenerology Specialists (consultation) | $25.00 |
| TOTAL OUT-OF-POCKET EXPENSES: | $4,707.26 | |
| Note that these costs do not include the cost of gas and wear and tear on my vehicle | ||
Regarding Insurance, Referrals, and Prior Authorizations
I'm not going into great detail here regarding insurance, referrals, and prior authorizations - that's a topic for another article. But let me say that I've had countless problems and delays over the past 4-5 years regarding this topic (yes, I have them all documented) and the bottom line for me is this:
There is something inherently wrong with the health care system in the United States.
I'm not talking about the fact that we seem to put too much emphasis on treatment and not nearly enough on prevention (even though that too is a problem).
I'm talking about the time and effort that I as a patient have had to invest (usually for routine things like an MRI, or approval to see a specialist) - not because I wanted to - but because I had to in order to get what I needed to have done in a timely fashion. It's beyond appalling, and I'm not exaggerating.
Even getting my November PET Scan to happen on time required an incredible number of phone calls and a near act of God (again, I'm not exaggerating, but I'm not going to use up any more time and energy to explain everything I had to do).
Something needs to change. Patients have ailments that are causing them pain or otherwise disrupting their lives. Patients shouldn't have to get involved in and expend energy on administrative issues. Their focus should be on what they need to do to get better and heal.
What an ordeal. The Miralax helps my mother a lot as she does 5 mg Oxycodone for severe spinal arthritis and severe scoliosis and it's constipation mitigation or crippling pain. Also does Sena but better results w/ Miralax. Plus your swallowing difficulties make Sena pills tough. ER on Saturday night is you, the drunks, ODs and gunshots.
My place is available to Linda. I believe you have a key. Was there for 20 minutes Wednesday on airport layover (Uber there and back) for urgent paperwork search. Toilet tank fills but flush handle chain inside tank needs reconnecting. Ran out of time.
Sheets and towels clean, just washed. As you know it's a "storage unit" and very disheveled. Welcome to stay.
Good call on ER even though huge wait.
NM does same thing Oregon does. However I believe you're going to pull through this. But it’s going to suck before it gets better.
Just updated through 12/6. You're excruciatingly detailed and thorough. Thanks for documenting this.
Spent time with Marie, breast cancer survivor from 2011. Double mastectomy. Whole deal was about 9 months. She recommends Flor Essence. Amazon. Marie and others have mentioned Colloidal Silver, at least 500 PPM, also on Amazon.
Will see Rob a stage 4 renal survivor, one year. Owns an Herb store, very knowledgeable. See him this weekend. Don't want to overload you w/Alternative therapies but trying for some cross references and consensus.
I have a vision of you hiking (briskly) so you can hit the gym, kick some ass on the chessboard and end the day playing guitar during sunset. The next morning you'll be loading up for a multi day camping and photo shoot journey. I don't believe our McDowell hike was your last in late October.
Yay you!! I knew you would make it through the simulation!
I'm very sorry to hear you didn't feel well over the weekend. I'm glad they tested you for the seasonal viruses and were negative. Maybe your body is reacting to your procedure last week with a low grade fever and it may have stimulated some extra saliva that you may not be swallowing properly.
I assume you had an IV during the procedure? If so is that site doing OK? We all react differently when our body is disturbed. Disease/medicine has some black and white areas but more grey than You'd think. You need to be diligent following and reporting symptoms. But it could be your body seeing the tube placement as an invasion it needs to attack. Have you checked out immunosuppression yet? As you do a great job as a researcher and recorder I would recommend you check it out.
I am sorry you are having to advocate for yourself so much. Do you have a case manager with your Medicare advantage? I would think they could help you. But healthcare is truly in crises. I empathize with what you're going through. I could share so much of my experience in that area but….. not now. It only elevates my blood pressure.
Thanks for updates through 11/24. Wonder if the feeding tube implant got infected (11/23). No doubt you checked. Any clarity on out of pocket this year and next? Are you able to amend your medicare during change/add window? Don’t know if you're "locked on" due to preexisting conditions. I'm a dumb-shit new to medicare 5/23. Needlessly complicated and cumbersome yet damn glad we have it. Making my own additions/changes 11/28 on phone consult.
How's that throat congestion from 11/24? Been able to keep lungs free after your 11/24 urgent care visit?
You're a brave man embarking on this aggressive treatment. Thank you for documenting all this; maybe very helpful for others.
Thanks for the update after 11/14. At least cancer hasn't spread. The feeding tube at least will get you the nutrients, medications, foods you need. At least Tramadol works on pain and is less addictive than say OxyContin. They have any idea how successful the 7 week chemo/radio protocol would optimally be?
Having lived in New Zealand on single payer national health. I know how good it can be. This was 25 years ago when we still had "good" options here. We had Mayo Platinum Plus available in Maricopa Co. only. There is nothing close to this in the U.S. today; even the old MPP we had then didn't compare to NZ national health around 2000. We are severely under resourced in U.S. health care today. Enough said.
Thank you for meticulous logging and documentation. Ive read this repeatedly, more than any other HWR post (and there are many great ones). Hopefully others will heed your remonstrations and assertively advocate for their health needs. You're the last person one would assume getting cancer. You have the cleanest, healthiest lifestyle I know of and stay on top of any ailments. The system failed you.
Where to from here? I have little idea what you're embarking on treatment wise. And I'm 2000 miles away. I'm imagining "It takes a Village" with local support to assist with domestic help, transport, moral support, general gal/guy Friday stuff. I send prayers and blessings but neither one of us puts great credence in that/those. As with any other huge life challenge it sucks going through this alone. My hope is somehow that a group of dear friends surrounds you and carts you along, especially with inevitable, incidental costs.
I'm hoping this blog post becomes a forum for this "village" for starters. I'm am open to all ideas and suggestions in how to help.